PPI-Antifungal Interaction Checker
Check Your Medication Combination
When you’re taking a proton pump inhibitor (PPI) for heartburn and suddenly need an antifungal for a stubborn yeast infection, things get complicated-fast. These two types of drugs don’t just sit quietly in your body. They bump into each other in ways that can make one or both stop working. And it’s not just a theory. Real patients are getting sick because their antifungals aren’t reaching the right levels in their blood. The problem isn’t always obvious, and many doctors still miss it.
Why PPIs Change How Antifungals Work
PPIs like omeprazole, esomeprazole, and pantoprazole shut down stomach acid production. That’s great if you have GERD, but terrible for certain antifungals. Drugs like itraconazole and ketoconazole need acid to dissolve properly. Without it, they can’t get absorbed into your bloodstream. Studies show that when you take a PPI with itraconazole, the amount of drug in your blood drops by 60%. That’s not a small drop-it’s enough to let fungal infections grow unchecked.
Think of it like this: your stomach is a gatekeeper. Normally, it opens the door for antifungals that need acid to pass through. PPIs slam that door shut. And once those antifungals can’t get in, they can’t reach the infection. That’s why the FDA added a black box warning to itraconazole in 2023: don’t take it with PPIs. The same warning applies to ketoconazole. Even if you feel fine, your body might not be getting enough medicine.
Fluconazole Is the Exception
Not all antifungals are affected the same way. Fluconazole doesn’t care about stomach acid. It dissolves easily in water, no matter how alkaline your stomach is. Its bioavailability stays steady at around 90%, even with a PPI running in the background. That’s why fluconazole is often the go-to choice when someone needs both an antifungal and a PPI. No need to space out doses. No need to switch medications. It just works.
But here’s the catch: fluconazole has its own problems. It doesn’t interfere with absorption, but it messes with your liver’s drug-processing system. It blocks an enzyme called CYP2C9, which is how your body breaks down blood thinners like warfarin. If you’re on warfarin and start fluconazole, your blood can become too thin-leading to dangerous bleeding. That’s why doctors often cut warfarin doses by 20-30% when fluconazole is added. It’s not an absorption issue, but it’s still a life-threatening interaction.
Voriconazole: The Complicated Middle Ground
Voriconazole is tricky. It doesn’t rely on stomach acid to get absorbed, so PPIs don’t hurt its uptake. But here’s where it gets strange: PPIs actually slow down how fast your body clears voriconazole. That’s because both drugs use the same liver enzyme, CYP2C19. When a PPI blocks it, voriconazole builds up in your blood. That sounds good-until it doesn’t. Too much voriconazole can cause hallucinations, liver damage, and vision problems. The Cleveland Clinic’s 2024 guidelines say you must check voriconazole blood levels within 72 hours of starting a PPI. If levels are too high, you’ll need to reduce the dose by 25-50%.
It’s a balancing act. Too little voriconazole? The infection wins. Too much? Your body starts to break down. And there’s no easy fix. You can’t just space out the doses. You need blood tests. You need monitoring. And not every hospital does it well.

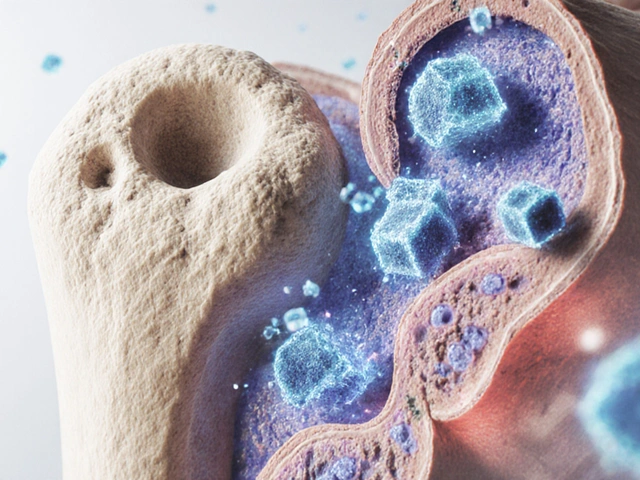
The Surprising Twist: PPIs Might Help Fight Fungi
Here’s where things get wild. A 2024 study found that PPIs might actually make some antifungals stronger-inside the fungus itself. Researchers discovered that omeprazole, the same drug that blocks stomach acid, also blocks a protein called Pam1p in Candida fungi. This protein helps the fungus pump out drugs like fluconazole. When PPIs block it, the fungus can’t get rid of the antifungal. The result? Fluconazole becomes 4 to 8 times more powerful against resistant strains of Candida glabrata.
This isn’t just lab magic. A clinical trial at Johns Hopkins is now testing whether adding omeprazole to standard fluconazole therapy can cure stubborn yeast infections that won’t respond to antifungals alone. If it works, we could be looking at a whole new way to treat drug-resistant fungal infections-using a common heartburn drug as a booster.
But here’s the catch: this effect only shows up in the fungus, not in your bloodstream. It doesn’t fix the absorption problem. You still can’t safely mix itraconazole with a PPI. But for fluconazole-resistant cases, adding a PPI might be the breakthrough we’ve been waiting for.
What Doctors Actually Do in Real Life
Despite the warnings, a 2024 audit found that over 22% of itraconazole prescriptions in the U.S. were still paired with PPIs. Why? Because doctors don’t always know. Or they think, “I’ll just give it anyway-maybe it’ll work.” But the data doesn’t lie. When itraconazole levels drop below 0.5 μg/mL, fungal infections don’t respond.
Top hospitals have clear protocols. UCSF says: if you must give itraconazole and a PPI, give the antifungal at least two hours before the PPI. Mayo Clinic recommends a 4-6 hour gap for ketoconazole. But even then, absorption still drops by 45%. That’s not enough. Most infectious disease pharmacists now say: don’t risk it. Switch to an echinocandin like caspofungin instead. It doesn’t care about stomach acid. It’s given by IV. It’s more expensive, yes-but it works.
And here’s the hidden cost: a 2024 study in JAMA Internal Medicine found that bad PPI-azole combinations lead to $327 million a year in extra hospital stays, repeat treatments, and complications. That’s not just a medical issue. It’s a financial one too.

What You Should Do If You’re on Both
If you’re taking a PPI and your doctor prescribes an antifungal, ask these questions:
- Which antifungal is it? (Ketoconazole? Itraconazole? Fluconazole? Voriconazole?)
- Is this the best choice given that I’m on a PPI?
- Will I need blood tests to check drug levels?
- Is there a safer alternative?
Don’t assume your doctor knows. Many don’t. And if you’re on fluconazole, ask about your blood thinner dose. If you’re on itraconazole, don’t take your PPI within two hours of it. Ever. And if you’re on voriconazole, make sure your pharmacy or hospital is checking your blood levels.
The Future: Better Drugs, Fewer Interactions
The good news? Scientists are working on solutions. A new form of itraconazole-called SUBA-itraconazole-is being tested. It uses tiny particles that dissolve without acid. In early trials, it delivered 92% of the drug into the bloodstream, no matter what the stomach pH was. If approved, this could make the PPI-itraconazole interaction a thing of the past.
And if the Johns Hopkins trial succeeds, we might soon be using omeprazole not just for heartburn, but as a tool to beat drug-resistant fungal infections. That’s the kind of twist that turns a problem into a breakthrough.
For now, though, the message is clear: don’t mix PPIs with itraconazole or ketoconazole. Fluconazole is safer-but watch for interactions with blood thinners. Voriconazole needs monitoring. And if you’re unsure, ask for help. Your life might depend on it.




8 Comments
I took itraconazole with omeprazole for 3 weeks and my yeast infection came back worse. My doctor said "it should be fine" lol. Turns out my blood levels were below 0.3. Now I’m on fluconazole and also taking a probiotic. Don’t trust your doctor blindly. I learned the hard way. 🤦♀️
Fluconazole and warfarin interaction is well documented. INR monitoring mandatory. No exceptions. PPIs reduce absorption of azoles requiring gastric acid. This is pharmacology 101. Why are we still having this conversation?
This is an exceptionally well-structured and clinically relevant summary. The distinction between absorption-dependent antifungals and those affected by hepatic metabolism is critical for safe prescribing. The emerging data on PPIs enhancing fluconazole efficacy within fungal cells via Pam1p inhibition represents a fascinating example of pharmacodynamic repurposing. I would be keen to see longitudinal outcomes from the Johns Hopkins trial, particularly regarding resistance development. The financial burden of avoidable hospitalizations due to these interactions further underscores the need for pharmacist-led medication reconciliation protocols in outpatient settings.
So let me get this straight. You’re telling me a $2 generic heartburn pill can turn a $500 antifungal into useless garbage… and doctors still don’t get it? And now we’re going to use the same pill to make the fungus *more* vulnerable? Sounds like someone’s been reading too much sci-fi. Meanwhile, my uncle’s still on omeprazole and ketoconazole because his PCP "didn’t think it mattered." We’re not fixing the system. We’re just slapping bandages on a hemorrhage.
This post gave me chills. Not because it’s scary-but because it’s so true. I’ve seen patients suffer because no one connected the dots. Please, if you’re reading this and you’re on a PPI: pause. Ask. Advocate. Your life isn’t a guessing game. And if your doctor doesn’t know the answer? Find someone who does. You deserve that.
Everyone’s acting like this is new. It’s not. The FDA warned about itraconazole and PPIs in 2008. People just ignore warnings until they get sick. And now we’re celebrating a 2024 study like it’s a miracle? The real miracle is that anyone still prescribes ketoconazole. It’s toxic. It’s outdated. And yes, I’m the guy who told you that in 2019. Still waiting for the rest of the world to catch up.
Bro I was on PPI for years and then got a fungal nail infection. Took fluconazole and it worked fine. No issues. But I also take a probiotic every day and drink ginger tea. Maybe that helped? Anyway if you’re worried just ask your pharmacist. They know way more than your doctor sometimes.
Suba-itraconazole is the future. The rest of this is just noise. If you’re still using ketoconazole, you’re practicing 1998 medicine. And if you’re not monitoring voriconazole levels, you’re gambling with neurotoxicity. This isn’t clinical care. It’s Russian roulette with a pharmacy label.