Warfarin-NSAID Bleeding Risk Calculator
Risk Assessment
Your Bleeding Risk
Specific Risks
Recommended Alternatives
- Acetaminophen (up to 3,000 mg/day) is generally safe with warfarin
- Topical NSAID gels/patches are much safer
- Physical therapy for joint/muscle pain
- Heat or cold therapy
When you’re on warfarin, even a simple pain reliever can turn dangerous. Many people don’t realize that common over-the-counter NSAIDs - like ibuprofen, naproxen, or diclofenac - can dramatically increase your risk of life-threatening bleeding when taken with warfarin. This isn’t a rare or theoretical concern. It’s a well-documented, clinically significant interaction that sends thousands to the hospital every year.
Why This Interaction Is So Dangerous
Warfarin works by blocking vitamin K, which your body needs to make clotting factors II, VII, IX, and X. Without these, your blood takes longer to clot - that’s the whole point if you’re on it for atrial fibrillation, a replaced heart valve, or deep vein thrombosis. But NSAIDs don’t work the same way. They stop your platelets from sticking together by inhibiting an enzyme called COX-1. Platelets are the first responders when you get a cut. If they can’t clump up, bleeding doesn’t stop easily.
Now imagine both happening at once: your blood can’t clot properly and your platelets are disabled. It’s not a 1+1=2 problem. It’s a multiplier effect. Studies show this combination can make bleeding risk more than four times higher than taking warfarin alone.
The Numbers Don’t Lie
A 2019 analysis from the European Society of Cardiology found that people taking warfarin and an NSAID together had a 2.09 times higher chance of bleeding compared to those on warfarin only. But not all NSAIDs are equal. Naproxen? It bumps up the risk by 4.1 times. Diclofenac? 3.3 times. Ibuprofen? Still dangerous - 1.79 times higher. Meloxicam, often thought to be safer, was linked to sharp INR spikes in one study - a sign your blood is thinning too much.
The bleeding isn’t just theoretical. It happens in real places:
- Stomach and intestines: 2.24 times higher risk of gastrointestinal bleeding
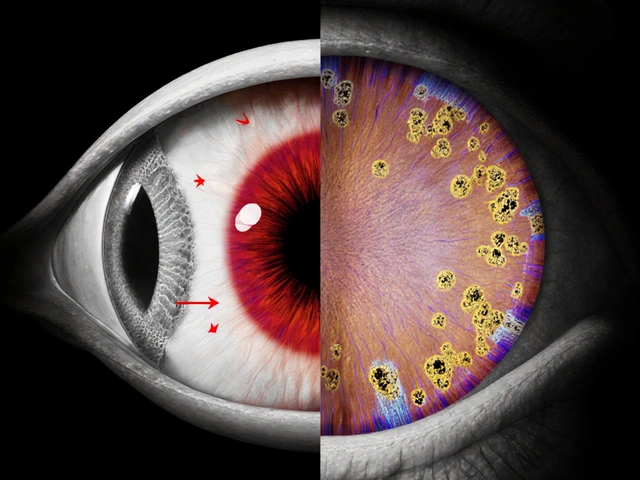
- Brain: 3.22 times higher risk of intracranial hemorrhage
- Lungs: 1.36 times higher risk
- Urinary tract: 1.57 times higher risk
And it’s not just bleeding. The same study found a near-tripling of anemia caused by slow, hidden blood loss. Many people don’t realize they’re bleeding internally until they’re dizzy, pale, or in shock.
Who’s at Highest Risk?
This isn’t a one-size-fits-all danger. Some people are far more vulnerable:
- Those on high-dose warfarin (over 40 mg per week) - their blood is already on the edge
- People taking other drugs that interact with warfarin - like antibiotics or antifungals
- Those with a low baseline INR - meaning their blood was clotting normally before the NSAID was added, so they have less room to absorb the extra thinning effect
One study of 98 warfarin users found that nearly 40% saw their INR jump by 15% or more after starting an NSAID. That’s not a small fluctuation. That’s a red flag requiring immediate medical attention.
It’s Not Just Warfarin
Even newer blood thinners like dabigatran or rivaroxaban aren’t safe with NSAIDs. While the risk isn’t quite as high as with warfarin, studies show NSAID users on these drugs still have significantly more major bleeding events - especially in the gut. One study found that 40% of major bleeds in NSAID users on direct oral anticoagulants happened in the digestive tract. So if you’re on any anticoagulant, assume NSAIDs are risky.
Why Your Stomach Is the First Target
NSAIDs don’t just mess with platelets. They also damage the stomach lining. They reduce prostaglandins - natural chemicals that protect your stomach from acid. Without them, your stomach is vulnerable to ulcers. Warfarin doesn’t cause ulcers, but if one forms, it bleeds more easily. That’s why gastrointestinal bleeding is the most common and deadliest outcome.
A 2024 meta-analysis confirmed: combining warfarin and NSAIDs doubles the risk of gastrointestinal bleeding compared to warfarin alone. Even selective COX-2 inhibitors, once thought to be gentler on the stomach, carry the same risk when paired with warfarin.
What You Should Do Instead
You don’t have to suffer in pain. There are safer options:
- Acetaminophen (paracetamol): Up to 3,000 mg per day is generally safe with warfarin. It doesn’t affect platelets or the stomach lining. It’s the first-line recommendation from major guidelines.
- Topical pain relievers: Gels or patches with NSAIDs like diclofenac applied to the skin (not swallowed) deliver pain relief with far less systemic effect. They’re much safer.
- Physical therapy: For joint or muscle pain, movement and strengthening can reduce reliance on pills.
- Heat or cold therapy: Simple, effective, and zero drug interaction risk.
If you absolutely must take an NSAID - say, after surgery or for severe arthritis - talk to your doctor. Use the lowest dose for the shortest time possible. Avoid naproxen and diclofenac if you can. Ibuprofen is less risky, but still dangerous. Always take it with food. And never skip your proton pump inhibitor (PPI), like pantoprazole, if it’s been prescribed to protect your stomach.

Monitoring Is Non-Negotiable
If you’re on warfarin and your doctor says you need an NSAID, INR checks become critical. Don’t wait for your next scheduled test. Get your INR checked within 3 to 5 days after starting the NSAID. Then check weekly until it stabilizes. A sudden rise in INR means your blood is thinning too fast. It’s not a lab result - it’s a warning sign.
Also, watch for symptoms: black or tarry stools, vomiting blood, unusual bruising, headaches that won’t go away, dizziness, or sudden weakness. These aren’t normal. Call your doctor immediately.
Why This Keeps Happening
Despite decades of evidence, this interaction is still common. A 2022 study found nearly 29% of warfarin users got at least one NSAID prescription in a year. Many patients don’t realize OTC painkillers count. Others assume their doctor knows about it. But doctors are busy. Pharmacists aren’t always consulted. The system fails.
This isn’t about blame. It’s about awareness. You’re the most important person in your own care. If you’re on warfarin, treat every NSAID - even a single tablet - like a potential threat.
The Bottom Line
Warfarin and NSAIDs don’t mix. The risk isn’t small. It’s real, measurable, and deadly. You don’t need to live in pain. There are safer ways to manage it. Acetaminophen, topical treatments, physical therapy - these aren’t second choices. They’re the right ones.
If you’re taking both, talk to your doctor today. Ask: Is this NSAID absolutely necessary? Is there a safer alternative? Have you checked my INR since I started this? Don’t assume it’s fine. Don’t wait for bleeding to happen. Prevention is the only safe strategy.





15 Comments
Man, I didn't realize ibuprofen could be this dangerous on warfarin. My dad's been popping Advil for his knees for years and just found out he's on warfarin for AFib. Scary stuff. Glad I read this before I gave him a pill for his back pain.
I'm a nurse and I see this all the time. Patients think 'OTC' means 'safe'-nope. I always ask about NSAIDs during med reconciliation. Even one tablet can spike INR. Acetaminophen is the real MVP here.
COX-1 inhibition + vitamin K antagonism = synergistic hemorrhagic cascade. The platelet dysfunction compounded with impaired coagulation factor synthesis creates a perfect storm for GI and CNS bleeding. This isn't just pharmacokinetics-it's pharmacodynamic dominoes.
Also, meloxicam’s off-label use in elderly patients is terrifying. That 2021 JAMA paper showed 37% of patients on warfarin + meloxicam had INR >5 within 72 hours. No one’s monitoring that.
And let’s not forget the PPI gap-only 22% of high-risk patients on this combo are prescribed one. That’s malpractice-tier negligence.
Wow. Someone actually wrote a comprehensive post without dumbing it down. Imagine that. Most people think 'warfarin' means 'don't eat broccoli' and call it a day. This? This is medical literacy. Kudos.
So you're saying I can't take Aleve for my back pain? What am I supposed to do, just suffer? This is why America's healthcare is broken-doctors scare people into inaction instead of giving real options.
TOPICAL NSAIDS ARE A GAME CHANGER. I’ve been using diclofenac gel for my arthritis and my INR hasn’t budged. Zero GI drama. Zero bleeding. Just chill pain relief. Why isn’t this the #1 recommendation?!
Also-heat wraps. Magic. I put one on before bed and sleep like a baby. No pills. No panic. Just warmth and peace.
As someone from India where NSAIDs are sold over the counter like candy, this is critical. My uncle took naproxen with warfarin for a week-ended up in ICU with GI bleed. He didn’t even know they interacted. We need public health campaigns, not just Reddit posts.
It’s funny how we treat medicine like a vending machine. Pop a pill, fix the problem. But the body isn’t a machine-it’s a web. Pull one thread, the whole thing trembles. Warfarin + NSAID isn’t just risky-it’s a metaphor for how we misunderstand biology.
THIS IS WHY WE NEED TO BAN NSAIDS FROM THE PHARMACY COUNTER. 🚫💊
People are dying because they think 'natural' means 'safe.' Ibuprofen isn't natural-it's a synthetic COX inhibitor that turns your blood into tap water. 🤦♂️
And don't get me started on meloxicam. That stuff is a silent killer for seniors. We need a national alert. #WarfarinAwareness
Acetaminophen is fine but it's not a panacea. Liver toxicity is real, especially in alcoholics. You're just swapping one risk for another. Why not just... accept pain? Maybe your body's trying to tell you something.
So what? People die from Tylenol overdoses too. You're acting like this is some secret government conspiracy. It's not. It's medicine. Risk is part of life.
I love how this post doesn’t just scare you-it gives you a path forward. Topical gels, PT, heat packs… these aren’t ‘alternative’ options. They’re smart, sustainable ones. Thank you for the hope, not just the horror.
And yet, we still treat pain like an enemy to be defeated, not a signal to be understood. Maybe the real issue isn’t the drug interaction-it’s our cultural refusal to sit with discomfort.
As a Canadian, I find it astonishing that such critical pharmacological information is not universally mandated in pharmacy counseling. In our system, every NSAID dispensed to a patient on anticoagulants requires a mandatory consultation with a clinical pharmacist. Why is this not standard in the U.S.?
INR >4.5 after NSAID? That’s not a fluctuation. That’s a code blue waiting to happen. Stop guessing. Check it. Now.