Blood Pressure Medication Safety Checker
Many women don't realize that common blood pressure medications like ACE inhibitors and ARBs can be dangerous during pregnancy. This tool helps you determine if your medication is safe during pregnancy and provides information about safe alternatives.
Important: If you're pregnant or planning pregnancy, consult your doctor before making any changes to your medication.
These medications are considered safe during pregnancy and are recommended for women with hypertension:
Labetalol - Beta-blocker, first-line choice. Starting dose: 100mg twice daily.
Methyldopa - Oldest and most studied option for pregnancy. Starting dose: 250mg twice daily.
Nifedipine - Calcium channel blocker, second-line option. Use extended-release form.
Result
Enter a medication name above to check its safety during pregnancy.
When a woman finds out she’s pregnant, everything changes-especially if she’s been taking medication for high blood pressure. Many women don’t realize that common drugs like ACE inhibitors and ARBs can seriously harm their unborn baby. These medications, often prescribed for decades to manage hypertension, are not just risky-they’re dangerous during pregnancy. And the damage isn’t always obvious at birth. It can show up as kidney failure, low amniotic fluid, or even stillbirth. The good news? There are safe, well-tested alternatives. You don’t have to choose between controlling your blood pressure and protecting your baby.
Why ACE Inhibitors and ARBs Are Dangerous in Pregnancy
ACE inhibitors (like lisinopril, enalapril, and captopril) and ARBs (like losartan and candesartan) work by blocking a system in the body called the renin-angiotensin-aldosterone system, or RAAS. This system helps regulate blood pressure. But in a developing fetus, RAAS plays a completely different role-it’s essential for forming the kidneys and producing amniotic fluid. When you block it during pregnancy, the baby’s kidneys can’t develop properly. That leads to a cascade of problems: too little amniotic fluid (called oligohydramnios), underdeveloped lungs, skull deformities, and sometimes, fetal death.
It’s not just about birth defects. A 2011 study published in Obstetrics & Gynecology International followed over 300 pregnancies where mothers took ACE inhibitors or ARBs. The results were clear: babies exposed to these drugs were born, on average, 350 grams lighter than those not exposed. Their gestational age was also shorter by nearly two weeks. And here’s the most shocking part-25.4% of those pregnancies ended in miscarriage, compared to just 12.3% in women with similar health conditions who weren’t taking these drugs.
Even more alarming? The risk doesn’t stop after the first trimester. Many people used to think it was safe to take these drugs early in pregnancy and stop once they knew they were pregnant. That’s false. A 2020 meta-analysis of 15 studies, published in Pharmacology Research & Perspectives, showed that even first-trimester exposure increases the risk of poor outcomes. There is no safe window.
ARBs vs. ACE Inhibitors: Which Is Worse?
Both classes are banned in pregnancy, but ARBs appear to be even more dangerous than ACE inhibitors. The American Heart Association’s 2012 review found that babies exposed to ARBs had worse outcomes-higher rates of kidney failure, longer hospital stays, and more neonatal complications. That’s why guidelines now treat them the same, but with extra caution for ARBs.
Specific drugs carry the most risk. For ACE inhibitors, enalapril, lisinopril, and ramipril are most commonly linked to problems. For ARBs, losartan and candesartan are the biggest concerns. The FDA labeled all of them as Pregnancy Category D-meaning there’s proven risk to the fetus. That’s the second-highest warning level, right below Category X (which means the drug should never be used in pregnancy). The European Medicines Agency and the World Health Organization have issued similar warnings. And yet, according to FDA data from 2021, about 1.2% of pregnancies in women with chronic hypertension still involve accidental exposure. That’s not because doctors are careless. It’s because patients often don’t know the risks until it’s too late.
What Should You Do If You’re Planning a Pregnancy?
If you’re taking an ACE inhibitor or ARB and thinking about getting pregnant, don’t wait. Talk to your doctor now. Switching medications before conception is the safest move. The American College of Obstetricians and Gynecologists (ACOG) recommends that women of childbearing potential who are on these drugs receive counseling about contraception and alternative treatments before they get pregnant. Many women don’t realize their blood pressure medication could affect their future pregnancy. They think, “I’ll stop it if I get pregnant.” But by then, the damage might already be done.
Healthcare providers should be asking: Are you planning a pregnancy? Are you using reliable contraception? If you’re not, then you need a safer medication. Some clinics now use checklists during routine visits to catch this before it becomes a crisis. The goal isn’t to scare you-it’s to prevent harm.
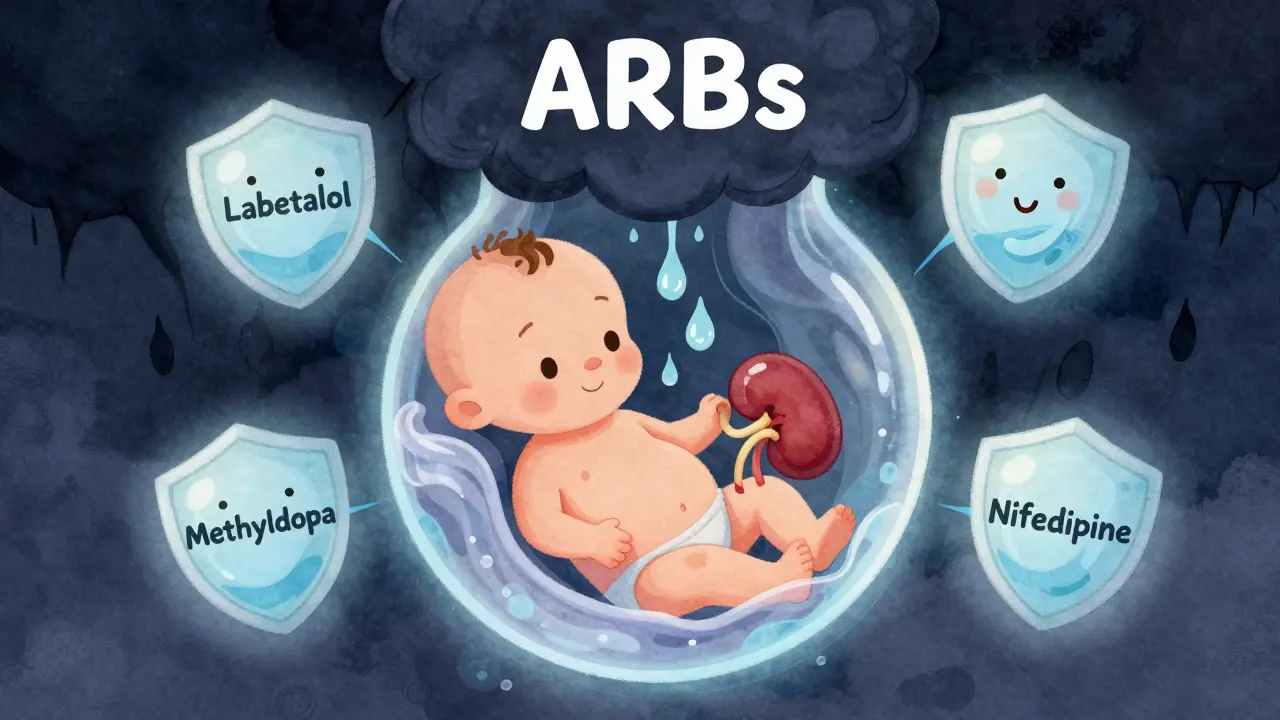
Safe Alternatives for Hypertension During Pregnancy
The good news? You have options. Three medications are widely recommended and proven safe for use during pregnancy:
- Labetalol: This beta-blocker is the go-to first-line treatment. It blocks both alpha and beta receptors, which helps lower blood pressure without affecting the baby’s heart rate or growth. It’s been used since the 1980s with excellent safety records. Starting dose is usually 100mg twice daily, and it can be increased up to 2,400mg per day if needed.
- Methyldopa: This is the oldest and most studied blood pressure medication for pregnancy. It’s been used since the 1970s. It works on the brain to reduce nerve signals that raise blood pressure. It’s taken as 250mg twice daily and can be increased up to 3,000mg per day. It’s especially good for women with mild to moderate hypertension.
- Nifedipine: A calcium channel blocker, nifedipine is often used as a second-line option. It’s especially helpful for sudden spikes in blood pressure. But it’s not ideal for women with heart conditions, as it can weaken the heart’s pumping ability. Extended-release forms are preferred to avoid rapid drops in pressure.
These drugs don’t just lower blood pressure-they do it without harming fetal development. Studies show babies born to mothers on labetalol or methyldopa have normal birth weights, normal amniotic fluid levels, and no increased risk of kidney problems. Blood pressure targets during pregnancy are the same as for non-pregnant adults: under 140/90 mmHg. But the goal isn’t just to hit numbers-it’s to keep both mother and baby healthy.
What If You’re Already Pregnant and Taking One of These Drugs?
If you’re pregnant and still taking an ACE inhibitor or ARB, stop immediately. Do not wait for your next appointment. Call your doctor today. Do not try to taper off on your own. The risks increase the longer you’re exposed. Your doctor will likely switch you to methyldopa or labetalol within 24 to 48 hours. In some cases, especially if your blood pressure is very high, you may need to be monitored in the hospital for a short time to ensure stability.
It’s not uncommon for women to feel guilty or anxious about this. But the truth is, this isn’t your fault. These drugs are often prescribed for years without warning. The system failed you-not you. The priority now is to act fast and safely.
What About Breastfeeding?
After delivery, the risks change. ACE inhibitors and ARBs are generally considered safe during breastfeeding, as very little passes into breast milk. But if you’re still on them postpartum, talk to your doctor about switching to a medication that’s safest for both you and your baby. Labetalol and methyldopa are still excellent choices if you need ongoing treatment. Many women stop blood pressure meds entirely after delivery, especially if their high blood pressure was pregnancy-related (like preeclampsia).
How to Prevent This From Happening to You
- Ask your doctor: “Is my blood pressure medication safe if I get pregnant?” Don’t assume it’s fine.
- If you’re on an ACE inhibitor or ARB and not using reliable contraception, ask about switching now.
- Keep a list of all your medications and share it with every provider you see.
- Use a pregnancy planner app or calendar to track your cycle and medication changes.
- If you’re trying to conceive, schedule a preconception visit with your OB-GYN or a maternal-fetal medicine specialist.
One simple conversation can prevent a lifetime of regret.
Can I take ACE inhibitors or ARBs if I’m trying to get pregnant?
No. Both ACE inhibitors and ARBs are strictly contraindicated during pregnancy, even before you know you’re pregnant. If you’re planning a pregnancy, switch to a safer alternative like labetalol or methyldopa at least three months before trying to conceive. Do not wait until pregnancy is confirmed.
Are there any safe blood pressure medications during pregnancy?
Yes. Labetalol and methyldopa are the two most recommended first-line options. Nifedipine is also considered safe and is often used as a second-line treatment. These medications have been studied for decades and show no increased risk of birth defects, low birth weight, or kidney problems in babies.
What happens if I accidentally take an ACE inhibitor during early pregnancy?
Stop the medication immediately and contact your doctor. While early exposure doesn’t always lead to complications, the risk of miscarriage, low amniotic fluid, and kidney issues increases. Your provider will likely order an ultrasound to check amniotic fluid levels and fetal kidney development. Close monitoring is essential.
Do ACE inhibitors cause birth defects?
They don’t always cause visible structural defects like heart or limb abnormalities. But they do cause serious functional damage-especially to the kidneys and lungs-by reducing amniotic fluid. This can lead to underdeveloped lungs, skull deformities, and kidney failure. These problems may not be obvious at birth but can be life-threatening.
Is it safe to switch from an ACE inhibitor to labetalol during pregnancy?
Yes. Switching to labetalol or methyldopa is the standard of care. Your doctor will monitor your blood pressure closely during the transition. Most women tolerate the switch well, and fetal outcomes improve significantly once the harmful medication is stopped.






11 Comments
Man, I wish I’d known this back when I was on lisinopril for my hypertension. I was trying to get pregnant and just assumed my doctor had my back. Turns out? They didn’t mention it at all. I switched to labetalol after a random Google deep dive and now I’m 32 weeks in with a healthy baby. No complications, no scare. Just a whole lot of relief. If you’re on an ACE/ARB and thinking about kids - don’t wait for the pregnancy test. Talk to your doc TODAY. Seriously.
Also, shoutout to the author for not just scaring people but giving real alternatives. That’s how you do public health.
Wow. So now we’re scaring women into switching meds based on a 2011 study? I’ve been on candesartan for 8 years. My BP is perfect. My kidneys are fine. My OB says I’m low risk. Why are we treating every pregnant woman like a ticking time bomb? This feels like fearmongering dressed up as care.
lol u all actin like aces r poison. my cousin took enalapril while preggo n her kid is 5 now n runs faster than me. u guys overreact. also methyldopa makes u feel like a zombie. i’d rather take my chances.
Okay but imagine being on ARBs and not knowing 😭
Like… I just found out my mom was on losartan when she got pregnant with me. I’m 28 and fine. But now I’m terrified my kidneys are secretly broken. 🤯
Also… labetalol gave me crazy fatigue. I went from ‘I can run a marathon’ to ‘I can’t make it to the fridge’. Anyone else??
This is one of those posts that makes you pause, exhale, and feel a weird mix of gratitude and horror. Gratitude because someone finally laid it out plain - no jargon, no fluff. Horror because so many women are walking around with these meds in their system like they’re vitamins.
What’s wild is how little we’re taught about reproductive pharmacology. We learn about birth control, sure - but not how the drugs we take for chronic conditions can silently sabotage a pregnancy before we even know it’s happening. This isn’t just medical advice - it’s reproductive justice.
And props to the author for naming the exact drugs that are risky. I’m gonna screenshot this and send it to my sister who’s on ramipril. She’s gonna need this.
So I switched to methyldopa at 8 weeks and honestly? It was harder than I thought. I kept forgetting to take it. My BP would spike and I’d panic. But I stuck with it. Now at 24 weeks, my numbers are stable and my ultrasound showed perfect amniotic fluid levels. If you’re scared to switch - just do it in small steps. Set phone alarms. Write it on your mirror. Tell your partner. You got this.
And if your doctor brushes you off? Find a new one. This is too important.
Thank you for writing this. I was one of those women who didn’t know. I found out I was pregnant and immediately stopped my ARB - then cried for three days because I thought I’d hurt my baby. I didn’t tell anyone. Felt so guilty.
But my OB was calm. Switched me to labetalol. Did the ultrasound. Everything looked fine. I’m 20 weeks now. I’m not perfect. But I’m alive. And so is my baby.
This post helped me feel less alone.
As someone from Australia, I’ve seen this play out in our public health system. We’ve got national guidelines that flag this risk, and pharmacists are trained to screen for it. But in rural areas? Still a gap. Women on long-term meds don’t always see an OB until they’re 16 weeks in. The real win here isn’t just the meds - it’s systemic change. We need preconception counseling built into primary care, not left to chance.
Also, labetalol is the MVP. My sister took it during both pregnancies. No issues. No drama. Just steady BP and happy babies.
So let me get this straight - we’re banning a whole class of meds because of a 25% miscarriage rate? What about the other 75%? Are those babies just lucky? Or are we ignoring confounding factors? What if the moms had worse BP control? What if they smoked? Had diabetes? This feels like correlation = causation with extra steps.
Also, methyldopa causes liver issues. Ever heard of that? No? Then you’re not doing the full research.
Just wanted to add something real quick - if you’re switching from an ARB to labetalol, don’t panic if your BP spikes a little at first. Your body’s adjusting. I went from 145/95 to 155/100 for two days. Scared me half to death. But my doc said it’s normal. After 72 hours, it stabilized. Just keep monitoring. And drink water. Seriously. Hydration helps more than you think.
Also - if you’re on nifedipine and feel dizzy? Sit down. Don’t drive. I learned that the hard way. 😅
It’s funny - we’ll spend hours debating whether a vaccine is safe for a 2-year-old, but when it comes to a pregnant woman on hypertension meds? We just assume she knows. Or that her doctor told her.
But here’s the truth: most people don’t even know what RAAS stands for. And that’s not their fault. It’s ours. The system’s failure. We’ve made medication management so fragmented - PCP, cardiologist, OB, pharmacist - no one’s talking.
What we need isn’t just better info. It’s a single, clear message: If you’re on an ACE/ARB and could get pregnant - switch now. No ifs. No maybes.
And if you’re reading this and you’re not pregnant? You might be soon. Be kind to your future self.