By 2026, nonalcoholic fatty liver disease affects nearly 1 in 4 people worldwide - and most don’t know it. Once called NAFLD, it’s now officially known as MASLD (metabolic dysfunction-associated steatotic liver disease), a name that better reflects what’s really going on: your liver is drowning in fat because of how your body handles sugar, fat, and insulin. This isn’t caused by drinking. It’s caused by being overweight, having high blood sugar, or struggling with cholesterol. And it’s quietly becoming the leading cause of chronic liver disease in the U.S., affecting over 100 million Americans.
What Actually Happens in Your Liver?
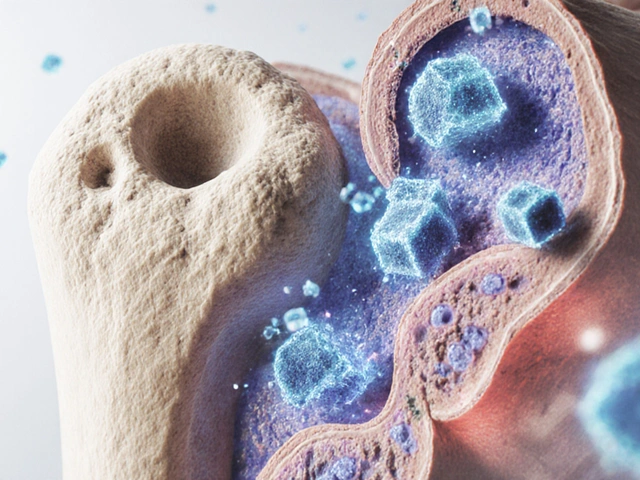
Your liver is your body’s main detox and metabolism hub. When you eat too many refined carbs and sugars - especially from soda, white bread, and processed snacks - your liver turns that extra glucose into fat. Normally, it sends that fat out as energy. But when you’re insulin resistant (a common condition in people with prediabetes or obesity), your liver gets overwhelmed. It starts storing fat instead of burning it. Over time, more than 5% of your liver cells fill up with fat. That’s MASLD.
At first, it’s just fat - called simple steatosis. Most people feel fine. But for about 20-30% of those with fat in their liver, inflammation kicks in. That’s now called MASH (metabolic dysfunction-associated steatohepatitis). Inflammation damages liver cells. Scar tissue builds up. This is fibrosis. Left unchecked, fibrosis turns into cirrhosis - a stiff, scarred liver that can’t work properly. In the worst cases, it leads to liver cancer or the need for a transplant.
Here’s the scary part: MASLD is now responsible for 24% of all liver transplants in the U.S. - up from just 5% in 2000. And unlike alcohol-related liver damage, there’s no quick fix. You can’t just quit drinking and heal. You have to fix your metabolism.
Who’s at Risk? The Real Culprits
If you have any of these, your liver is at risk:
- Waist size over 40 inches (men) or 35 inches (women)
- Type 2 diabetes or prediabetes
- Blood pressure over 130/80
- Triglycerides above 150 mg/dL
- Low HDL (‘good’ cholesterol) under 40 mg/dL (men) or 50 mg/dL (women)
These five things together are called metabolic syndrome. And if you have three or more, your chance of having MASLD jumps to 80%. Even if you’re not overweight, you can still have it - especially if you’re sedentary or eat a lot of fructose (found in sweetened drinks and processed foods).
Some groups are hit harder. Hispanics have the highest rates - nearly 45% - while non-Hispanic Blacks have lower rates, around 20%. But the fastest-growing group? Kids. One in 10 children now has fatty liver. In obese kids, it’s as high as 70%. That’s not normal aging. That’s a warning sign for an entire generation.
Why It’s So Hard to Diagnose
Most people with MASLD feel fine. No pain. No jaundice. No symptoms until it’s advanced. That’s why doctors often miss it. Liver enzymes (ALT and AST) can be normal even when fat is building up. Many patients are told their elevated liver enzymes are ‘just a fluke’ or ‘not serious.’
According to the American Liver Foundation, it takes an average of 3.2 years from when symptoms first appear to when MASLD is actually diagnosed. By then, some damage may already be done.
The gold standard test is a liver biopsy - but it’s invasive and carries small risks. That’s why doctors now use non-invasive tools like FibroScan, which measures liver stiffness. But insurance often denies coverage for these tests, even though AASLD guidelines recommend them. Many patients are stuck waiting or paying out of pocket.

The Good News: You Can Reverse It
Here’s the truth: if you catch MASLD early, you can reverse it - without drugs. In fact, 90% of simple steatosis cases improve with lifestyle changes. The key? Weight loss.
Research from UC San Diego shows:
- Losing 5-7% of your body weight reverses fat buildup in 81% of people
- Losing 10% resolves inflammation (MASH) in 45% of cases
- Keeping off that weight for 12 months cuts disease progression risk by 67%
You don’t need to become a fitness guru. You don’t need to go keto or vegan. You need to make two changes: eat less processed food, and move more.
How to Prevent and Reverse MASLD: Practical Steps
1. Cut Out Sugary Drinks and Refined Carbs
Soda, energy drinks, sweetened coffee, fruit juice - these are the biggest drivers of liver fat. A single 20-ounce bottle of soda has 65 grams of fructose. That’s more than your liver can handle in one go. Replace them with water, unsweetened tea, or sparkling water with lemon.
Swap white bread, pasta, and rice for whole grains, legumes, and vegetables. Foods with a low glycemic index (under 55) keep your blood sugar stable and reduce fat storage in the liver.
2. Eat a Mediterranean-Style Diet
Studies from the LiverLife App community show a 76% success rate in improving liver health with this approach:
- Fruits, vegetables, nuts, seeds
- Whole grains like oats and quinoa
- Fatty fish (salmon, mackerel) twice a week
- Olive oil as your main fat
- Lean protein like chicken, beans, tofu
- Minimal red meat, no processed meats
This isn’t a diet - it’s a way of eating that’s been proven to reduce liver fat, lower inflammation, and improve insulin sensitivity.
3. Move Every Day - Even Just a Little
You don’t need to run a marathon. Aim for 150 minutes a week of moderate activity - that’s 30 minutes, five days a week. Brisk walking counts. Gardening counts. Dancing around your kitchen counts.
Studies show people who hit 10,000 steps a day reduce liver fat by 30% in six months. Even if you’re overweight, moving regularly helps your liver burn fat instead of storing it.
4. Lose Weight - But Do It Slowly
Crash diets make MASLD worse. Rapid weight loss can trigger liver inflammation. Aim for 1-2 pounds a week. That’s sustainable. That’s safe.
Use a simple formula: cut 500 calories a day from your current intake. That’s one less sugary snack, one smaller portion of pasta, no dessert three nights a week. Combine that with movement, and you’ll lose weight without feeling deprived.
5. Get Screened - Even If You Feel Fine
If you have any of the risk factors above, ask your doctor for a liver enzyme test (ALT). Normal levels are under 30 U/L for women and under 40 U/L for men. If they’re high, push for a FibroScan or ultrasound. Don’t wait for symptoms.
And if you’ve been told your liver enzymes are ‘normal’ but you’re still worried - get a second opinion. Many patients with MASLD had normal enzymes early on.
What About Medications?
As of March 2024, the FDA approved the first drug for MASH: resmetirom. It’s not a cure. It reduces fibrosis progression by 24% compared to placebo. But it’s only for people with advanced disease and isn’t meant to replace lifestyle changes.
There are no other FDA-approved drugs yet. Supplements like vitamin E or omega-3s show mixed results and aren’t recommended as primary treatment. The truth? The only proven, powerful, and free treatment is still weight loss, better food, and daily movement.

Why This Matters Beyond Your Liver
MASLD isn’t just a liver problem. It’s a sign your whole metabolism is out of balance. People with MASLD have a much higher risk of heart disease, stroke, and type 2 diabetes. Fixing your liver means fixing your heart, your blood sugar, and your energy levels.
Companies like IBM have seen a 37% drop in MASLD cases among employees after launching workplace wellness programs focused on nutrition and activity. That’s not just health - it’s productivity, fewer sick days, and lower insurance costs.
What Comes Next?
By 2030, half of all U.S. adults will be obese. If nothing changes, MASLD could affect 35% of the global population by 2040. That’s not a future prediction - it’s a current trend.
But here’s the flip side: MASLD is one of the few chronic diseases we can actually prevent - even reverse - with simple, everyday choices. No magic pills. No expensive surgeries. Just better food, more movement, and a little patience.
If you’re reading this and you’re worried about your liver - you’re already ahead of most people. The next step? Talk to your doctor. Get tested. Start small. One less soda. One extra walk. One healthier meal. That’s how you take back your health - one day at a time.
Can you have fatty liver without being overweight?
Yes. While obesity is the biggest risk factor, people with normal weight can still develop MASLD - especially if they have insulin resistance, high triglycerides, or eat a lot of sugar and refined carbs. This is sometimes called ‘lean MASLD’ and makes up about 10-20% of cases. It’s often missed because doctors assume only overweight people are at risk.
Does alcohol cause MASLD?
No. MASLD is defined by the absence of significant alcohol use. But drinking alcohol - even in small amounts - can make MASLD worse. The American Association for the Study of Liver Diseases recommends complete abstinence, while some European guidelines allow up to 30 grams per day. To be safe, avoid alcohol if you have MASLD. It adds stress to your liver and speeds up scarring.
Can children get MASLD?
Yes. Pediatric MASLD is rising fast. Around 1 in 10 children in the U.S. now have it, and up to 70% of obese children are affected. It’s often linked to sugary drinks, processed snacks, and lack of physical activity. Early detection through liver enzyme tests is critical - the earlier you intervene, the better the chance of reversal.
Is a liver biopsy always needed to diagnose MASLD?
No. While a biopsy is the most accurate test, it’s not always necessary. Doctors often use blood tests, FibroScan (a painless ultrasound), or MRI-PDFF to detect fat and fibrosis. Biopsies are usually reserved for cases where the diagnosis is unclear or when advanced fibrosis is suspected. Non-invasive tests are now recommended as first-line tools by major liver societies.
How long does it take to reverse fatty liver?
For simple steatosis, you can see improvements in liver fat within 3-6 months of losing 5-7% of your body weight and making dietary changes. MRI scans show fat reduction by 30% or more in that time. Reversing inflammation (MASH) takes longer - often 12 months or more - and requires sustained weight loss of 10% or more. The key is consistency, not speed.
Can MASLD lead to liver cancer?
Yes. If MASLD progresses to cirrhosis, the risk of hepatocellular carcinoma (liver cancer) increases significantly. Even without cirrhosis, people with MASH have a higher risk than those with simple steatosis. That’s why early intervention is so important. Preventing fibrosis is the best way to avoid cancer down the road.
Are there any supplements that help?
Some studies show vitamin E may help in non-diabetic adults with MASH, but it’s not recommended for everyone due to potential risks. Omega-3s can lower triglycerides but don’t reliably reduce liver fat. Coffee consumption is linked to lower liver fibrosis risk - drinking 2-3 cups a day may help. But no supplement replaces weight loss, diet change, and exercise. Always talk to your doctor before taking anything.
What to Do Next
If you’ve been told you have fatty liver - or if you have any of the risk factors - start here:
- Get your ALT and AST levels checked.
- Measure your waist. If it’s over 35 inches (women) or 40 inches (men), that’s a red flag.
- Track your sugar intake for one week. Cut out sugary drinks and snacks.
- Start walking 30 minutes a day, five days a week.
- Ask your doctor about a FibroScan or ultrasound - don’t wait for symptoms.
You don’t need to fix everything at once. One change leads to another. And when your liver gets healthier, you’ll feel it - more energy, clearer thinking, better sleep. This isn’t about looking different. It’s about living longer - and better.





8 Comments
So basically, if I stop chugging Mountain Dew and start walking to the fridge instead of rolling to it, my liver might not turn into a greasy pizza crust? 😅
Also, 70% of obese kids have this? That’s not a health crisis-that’s a fast-food commercial starring my nephew. 🍔💔
I’m from a culture where meals are shared, not consumed in isolation-and our liver health reflects that. My abuela cooked with olive oil, fresh herbs, and zero processed sugar. No pills. No scans. Just food that remembers its roots.
Maybe the real cure isn’t in the lab-it’s in the kitchen, passed down like a recipe. 🌿🫶
While the data presented is compelling and aligns with current clinical guidelines, I find the framing of ‘no magic pills’ slightly reductive. The approval of resmetirom represents a significant milestone-not as a replacement for lifestyle, but as an adjunct for those already in advanced stages.
It’s worth acknowledging that metabolic dysfunction is systemic, and while behavioral change is foundational, denying pharmacological progress risks alienating patients who need more than willpower to survive.
Let’s cut the fluff: your liver is a goddamn trash compactor for your sugar addiction. Soda? That’s not a drink-it’s liquid betrayal. White bread? That’s just sugar with a bread costume.
And yeah, you don’t need to become a CrossFit warrior. Just stop eating like a raccoon in a 7-Eleven. Walk more. Eat real food. Sleep like a human. Your liver will throw you a parade. Or at least stop screaming in silent, fibrotic agony.
Also-get a FibroScan. Insurance be damned. Your future self will high-five you.
I appreciate how this post avoids fearmongering while still underscoring urgency. The fact that MASLD can be reversed without medication is both empowering and humbling.
It reminds me that health isn’t about perfection-it’s about persistence. One less soda. One extra block walked. One meal cooked at home. These aren’t grand gestures, but they’re the quiet revolutions that rebuild bodies-and lives.
But… what if… the real issue isn’t sugar… or fat… or insulin… but the existential alienation of modern life? We’re not just overeating-we’re over-obsessing, over-scheduling, over-stimulating… and our livers? They’re just the collateral damage of a civilization that forgot how to breathe, how to rest, how to be…
And yes, I know it’s trendy to say ‘just lose weight’-but what if weight is just the symptom of a soul that’s been starved of meaning? I mean… have you ever truly sat with your liver? I mean… really sat? And asked it… what it needs?
…I’ve cried into my kombucha about this. Twice.
I just got my FibroScan results yesterday. 8.2 kPa. My doctor said ‘mild fibrosis.’ I cried in the parking lot.
Then I went home, threw out my soda stash, and walked 12,000 steps while listening to my 8-year-old recite the entire Frozen 2 soundtrack.
It’s not glamorous. It’s not viral. But it’s mine.
And for the first time in years… my liver feels like it’s breathing too.
Interesting framework, though I’d argue the term ‘metabolic dysfunction’ is a semantic obfuscation-essentially rebranding ‘obesity-related hepatic steatosis’ to depoliticize the systemic failures of food policy, agricultural subsidies, and urban food deserts.
Individual agency is a convenient myth when the environment is engineered for metabolic collapse. The ‘two changes’ solution is elegant, but it ignores that not everyone has access to olive oil, a safe walking path, or the luxury of time.
…Also, I’m pretty sure I ate a Pop-Tart yesterday. Oops. 😅