When your doctor prescribes a medication, they expect you to take it. But what happens when you don’t? For decades, doctors called it compliance-as if patients were machines that needed to be programmed correctly. Today, that language is outdated. The real issue isn’t whether you’re following orders. It’s whether you’re adherent-and why that difference changes everything.
Adherence Isn’t Just About Taking Pills
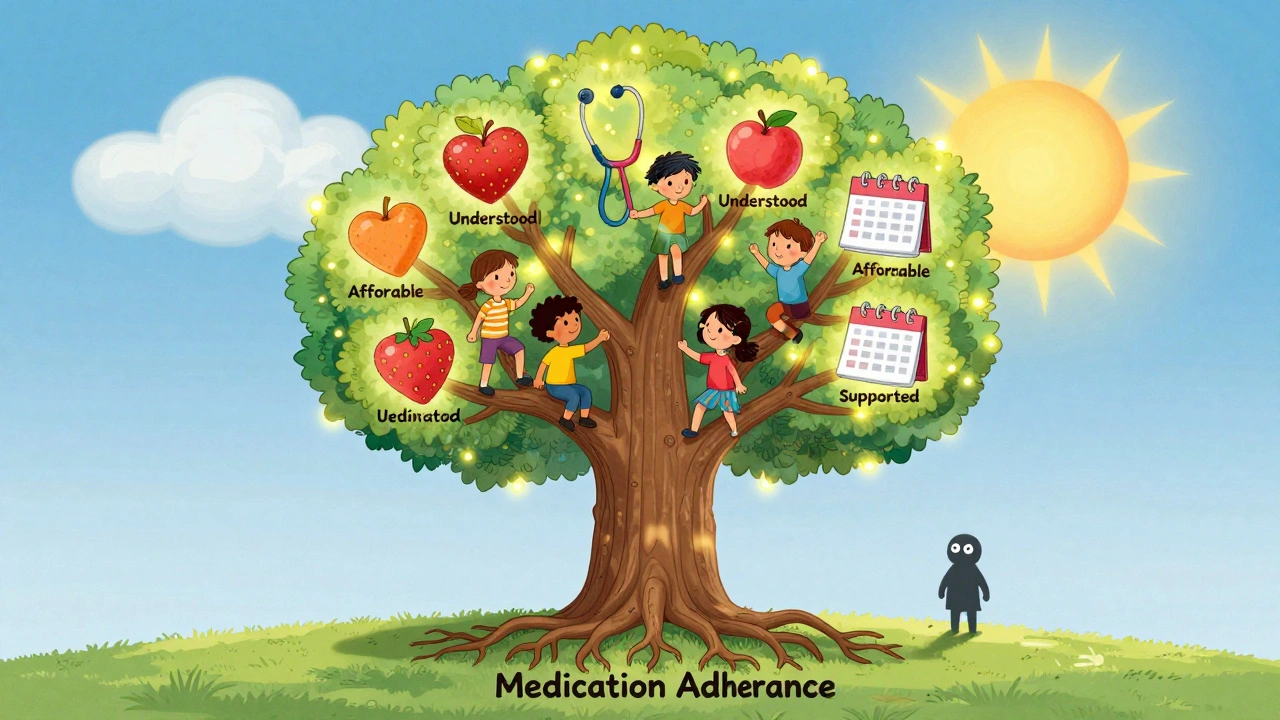
Medication adherence means you’re actively participating in your own care. It’s not just about swallowing pills on time. It’s about understanding why you’re taking them, managing side effects, adjusting your schedule, and deciding-alongside your provider-what works for your life. The American Pharmacists Association defines it as how closely your behavior matches the treatment plan you agreed to. Not what was ordered. What you agreed to.
That’s a huge shift. Adherence recognizes that you’re not a passive recipient. You’re a person with a job, a family, money worries, side effects, cultural beliefs, and daily routines. Maybe you skip a dose because the pill makes you dizzy. Maybe you can’t afford it. Maybe you think your blood pressure is fine now, so you don’t need it anymore. Adherence doesn’t label you as ‘non-compliant.’ It asks: What’s getting in your way?
Compliance Is Old-School Control
Compliance is the old way. It’s a one-way street: doctor gives instructions. Patient follows. If you don’t, you’re seen as disobedient. No questions asked. No context considered.
Think of tuberculosis treatment. In hospitals, nurses watch patients swallow every pill-called directly observed therapy (DOT). That’s compliance. It works because the condition is serious, the treatment is short, and the setting is controlled. But for high blood pressure, diabetes, or cholesterol? That model collapses. Most people take meds for years, sometimes for life. You can’t have a nurse watching you every morning.
And here’s the problem with compliance language: it blames you. If you miss doses, you’re ‘non-compliant.’ That makes you feel guilty, ashamed, or defensive. It shuts down conversation. It doesn’t help you stay on track-it just labels you.
Why the Shift Happened
The change from compliance to adherence didn’t happen overnight. It started in the 1990s as healthcare began focusing on patient-centered care. The American Medical Association, the FDA, and the World Health Organization all pushed for language that respected patient autonomy.
By the early 2000s, major journals like the Annals of Internal Medicine and the Journal of Clinical Pharmacy and Therapeutics stopped using ‘compliance’ in research. Why? Because studies showed it didn’t predict outcomes. People who were labeled ‘non-compliant’ weren’t necessarily ignoring advice-they were struggling with real barriers: cost, confusion, side effects, depression, or lack of support.
Dr. Robert H. Brook, a leading expert from UCLA, called the shift from compliance to adherence ‘one of the most significant conceptual advances in patient care over the past three decades.’

How Adherence Is Measured (And Why It’s More Accurate)
Compliance used to be measured by counting pills or checking refill records. Did you pick up your prescription? Good. You’re compliant.
Adherence uses smarter tools:
- Medication Possession Ratio (MPR): If you’ve got enough pills for 80% or more of the days you should be taking them, you’re considered adherent. That’s the standard set by the AMA.
- Electronic caps: Some pill bottles have chips that log when you open them. This shows not just if you took the pill, but when-and whether you’re taking it at the right time.
- Self-reporting: Simple questions like ‘How often do you miss doses?’ give real insight when asked without judgment.
- Pharmacy data: Are you refilling your statins every 30 days? Or letting them run out for months?
Adherence also tracks three phases:
- Initiation: Did you start the medication at all?
- Implementation: Are you taking it correctly-right dose, right time?
- Discontinuation: When and why did you stop?
Compliance only looks at phase two. Adherence sees the whole picture.
What Happens When People Don’t Adhere
Half of all patients stop taking their meds within the first year. That’s not laziness. That’s the system failing them.
For people with high blood pressure, skipping doses means higher risk of stroke. For diabetics, it means nerve damage, kidney failure, or amputations. For heart failure patients, it leads to hospital readmissions-costing the U.S. healthcare system over $100 billion a year.
The World Health Organization estimates that poor adherence causes 125,000 deaths annually in the U.S. alone. That’s more than traffic accidents.
And here’s the kicker: most of these deaths are preventable. Not because patients are bad. But because care models are outdated.
What Works: Adherence-Focused Care
Healthcare providers who use adherence strategies see big improvements:
- Patients who get motivational interviewing-a conversation style that helps them explore their own reasons for taking meds-show 37.6% higher adherence rates.
- Tools like Hero Health and Dose Packer use smart dispensers and reminders. One Kaiser Permanente study found missed doses dropped by 42%.
- Pharmacists who spend 10-15 minutes reviewing meds with patients-instead of just handing out prescriptions-see patients stick with treatment longer.
It’s not about more pills. It’s about better conversations.
Providers now need training-not just in medicine, but in communication. The American Academy of Family Physicians says it takes 8-12 hours of special training to do this right. But the payoff? Fewer ER visits, lower costs, and real health improvements.
Technology Is Making Adherence Smarter
AI is stepping in. Google Health’s 2024 study showed machine learning can predict who’s likely to miss doses-with 83.7% accuracy-by looking at 27 factors: income, zip code, past refill patterns, side effect reports, even weather changes.
That means a system can flag a patient who hasn’t refilled their blood pressure med in 45 days, then automatically send a text: ‘Hey, we noticed you haven’t picked up your meds. Want to talk about what’s going on?’
The FDA and EMA now require adherence data in clinical trials. The AMA added new billing codes in 2025 for adherence counseling (99487-99489). Hospitals now get paid more if patients stay on their meds.
By 2028, the global market for adherence tools will hit $11.7 billion. That’s not because companies are pushing gadgets. It’s because the evidence is undeniable: adherence saves lives and money.
Why This Matters to You
If you’re on medication, this isn’t just a clinical term. It’s about your life.
You don’t have to be ‘compliant.’ You don’t have to feel guilty for forgetting a pill. You don’t have to hide that you can’t afford it. You have the right to say: ‘This doesn’t work for me.’
And your provider should listen-not judge.
Adherence means you’re part of the team. Your voice matters. Your schedule matters. Your budget matters. Your fears matter.
When you feel heard, you’re more likely to stick with treatment. When you’re blamed, you shut down.
What’s Next
By 2035, McKinsey & Company predicts 95% of healthcare systems will require adherence-based care. It’s not optional anymore. It’s the standard.
And it’s not just about pills. It’s about dignity. It’s about respect. It’s about recognizing that healing isn’t about obedience-it’s about partnership.
If you’re on medication, ask your provider: ‘What’s the plan for helping me stay on track?’ If you’re a provider, ask yourself: ‘Am I asking why they’re struggling-or just counting missed doses?’
The answer changes everything.
What’s the difference between medication adherence and compliance?
Medication compliance means following a provider’s instructions without question, like a machine. Adherence means actively participating in your care-you understand the plan, agree to it, and make it work with your life. Adherence respects your choices; compliance blames you for not obeying.
Is adherence better than compliance?
Yes. Adherence leads to better health outcomes because it addresses real barriers like cost, side effects, and lifestyle. Studies show adherence-focused care improves treatment success by 20-50% compared to compliance-only approaches. It also reduces hospital visits and saves money.
How do I know if I’m adherent?
You’re considered adherent if you take at least 80% of your prescribed doses over time. But it’s not just about numbers. Ask yourself: Do I understand why I’m taking this? Can I afford it? Do I have support? Are side effects manageable? If yes, you’re likely adherent-even if you miss a dose now and then.
Why do people stop taking their meds?
The top reasons: side effects (like dizziness or nausea), cost (meds are too expensive), forgetfulness, thinking they’re fine now, or not understanding how the drug works. It’s rarely about being lazy or rebellious.
What can I do if I’m struggling to take my meds?
Talk to your provider or pharmacist. Don’t hide it. Ask for help: Can we switch to a cheaper drug? Can I get a pill organizer? Can we adjust the schedule? Many clinics now offer adherence counseling-sometimes covered by insurance. You’re not failing. You’re human.
Are there tools to help with adherence?
Yes. Smart pill dispensers like Hero Health, reminder apps, blister packs, and pharmacy refill alerts help. Some systems even text you if you miss a dose. Ask your provider if they use any of these tools-or if they can connect you with one.
Why do some providers still use the word ‘compliance’?
Old habits die hard. Some providers were trained in the old system. Others work in settings like prisons or emergency care, where compliance language still persists. But major health systems, the FDA, and the AMA have all moved to adherence. The shift is happening-just not everywhere yet.
Can adherence really prevent deaths?
Yes. The WHO estimates adherence-focused care could prevent 850,000 premature deaths annually in low- and middle-income countries by 2030-and 150,000 in high-income countries. Most of those deaths are from heart disease, diabetes, and hypertension-conditions that are manageable if meds are taken consistently.






13 Comments
I skip doses when I'm broke or dizzy. No shame. Just life.
This is the kind of shift healthcare needs. Not more pills. More listening. I've seen patients light up when their pharmacist asks, 'What's making this hard?' instead of 'Why'd you miss your dose?' It's not about obedience. It's about partnership. And honestly? That's how healing starts.
The terminology shift from compliance to adherence is not semantic fluff-it's a fundamental reorientation of power dynamics in clinical relationships. The language we use shapes our assumptions. 'Compliance' implies hierarchy. 'Adherence' implies collaboration. This isn't just political correctness; it's evidence-based care.
I work in rural Ireland and we see this every day. People skip meds because the pharmacy is two hours away or the co-pay is more than their lunch. No one’s lazy. The system just doesn’t fit. Adherence means designing care around real lives-not forcing lives to fit the care.
Oh wow. So now we're calling people 'adherent' instead of 'non-compliant' and magically their blood pressure drops? Funny how the same people who call this 'patient-centered care' also want to ban sugar and mandate 8 hours of sleep. If you really cared, you'd fix the $1200 insulin. Not rename the problem.
This is what happens when you let soft liberals run medicine. People don't need empathy. They need discipline. If you can't take a pill, you don't deserve to live. This is why America is dying.
Adherence is just a euphemism for obedience. Same thing. Different word.
My grandma takes 12 pills a day. She forgets half. But she laughs when her pill box beeps. We got her one with a little light. She says it’s like her little robot buddy. No judgment. Just help. Works better than any lecture.
In India, we don't need Western buzzwords. We know discipline. We know sacrifice. People here take their medicine because they know it's their duty. This 'adherence' nonsense is just another American excuse for weakness.
I work in a pharmacy in Delhi. We give free reminders via WhatsApp. We ask patients what time they eat, sleep, work. Then we match the pill schedule. No one says 'non-compliant' here. We just help. And guess what? More people stick with it. Simple.
This isn't just about pills-it's about dignity. When you treat someone like a malfunctioning robot, they become one. But when you ask them what’s blocking them? When you listen? Magic happens. I’ve seen people restart insulin after a 2-year break because their pharmacist didn’t shame them. That’s not medicine. That’s humanity.
Adherence is a con. It lets patients off the hook. They’re still failing. You just made them feel better about it. That’s not healthcare. That’s therapy with a stethoscope.
If you can't follow simple instructions, you shouldn't be on meds. End of story.