It’s January 2026, and COVID-19 isn’t gone - it’s just different. You won’t hear about lockdowns or empty grocery shelves anymore. But if you’ve had a bad cold this winter that just wouldn’t quit, or if your neighbor’s kid missed two weeks of school with a throat so sore they couldn’t swallow, you’re likely dealing with the latest version of SARS-CoV-2. The virus has evolved. So have the vaccines. And so should your understanding of what’s going on.
What Symptoms Are You Actually Facing?
The old list of COVID-19 symptoms - fever, cough, loss of taste - doesn’t tell the whole story anymore. Today’s dominant variant, XFG (also called Stratus), hits differently. People report congestion, a scratchy or stabbing sore throat, headache, muscle aches, and fatigue. It doesn’t always start with a fever. Sometimes, it starts with a cough that won’t go away or a headache that feels like pressure behind the eyes.
Another variant, Nimbus, has been linked to that sharp, sudden throat pain - the kind that makes you wince when you swallow. It’s not unique to one strain, but it’s common enough that doctors now ask patients: “Did your sore throat come on fast and feel like a knife?” If yes, it’s worth testing.
And then there’s the long tail. About 1 in 5 people who’ve had COVID-19 still deal with symptoms three years later. Fatigue. Brain fog. Trouble sleeping. Shortness of breath after walking up stairs. These aren’t “just in your head.” They’re real, documented, and increasingly recognized by doctors as part of long COVID. Hospitalized patients are at higher risk, but even mild cases can lead to lingering issues.
What Variants Are Actually Circulating?
Forget the names you heard in 2021 - Alpha, Delta, even the original Omicron. They’re gone. As of October 2025, XFG (Stratus) makes up 85% of all cases in the U.S. The rest? NB.1.8.1 at 7%, and NW.1 at 3%. These aren’t random mutations. They’re the result of the virus adapting to our immune defenses - especially after billions of infections and vaccines.
What makes XFG so widespread? It spreads faster than earlier versions. It doesn’t necessarily make you sicker, but it’s better at slipping past immunity. That’s why so many vaccinated people still get infected - not because the vaccines failed, but because the virus changed. Dr. Mark Rupp from Nebraska Medicine puts it plainly: “We have a lot of disease out there. People should continue to be careful.”
And while XFG dominates now, surveillance is ongoing. The CDC and global health agencies track every new mutation. The next big one could emerge anytime - which is why vaccine updates happen every year.
Which Vaccines Work Right Now?
The 2024-2025 vaccines were updated to target KP.2, a strain that was common in early 2024. Pfizer and Moderna’s shots are built for KP.2. Novavax’s vaccine targets JN.1, but lab studies show it also works well against KP.2 and KP.3. That’s important - because even if your shot doesn’t match the exact variant, it still gives you protection.
And here’s the key point: the goal isn’t to stop every infection. It’s to stop you from ending up in the hospital. Studies from Ohio State University Health show the vaccines are strongest in the first three months after getting them. After that, protection against infection drops - but protection against severe illness stays high.
For the 2025-2026 season, the FDA approved a new formula in May 2025 based on variants circulating in spring and summer 2025. The CDC recommends everyone 6 months and older get an updated shot every year. If you had COVID recently, wait at least three months after your symptoms started - or after your positive test if you were asymptomatic - before getting the new vaccine.
Side effects? Most people report nothing. Of the 1,245 people surveyed in June 2025, 87% had mild or no side effects. The most common? Fatigue (32%), sore arm (28%), and headache (19%). No one’s dying from the vaccine. But thousands are still being hospitalized because they didn’t get it.
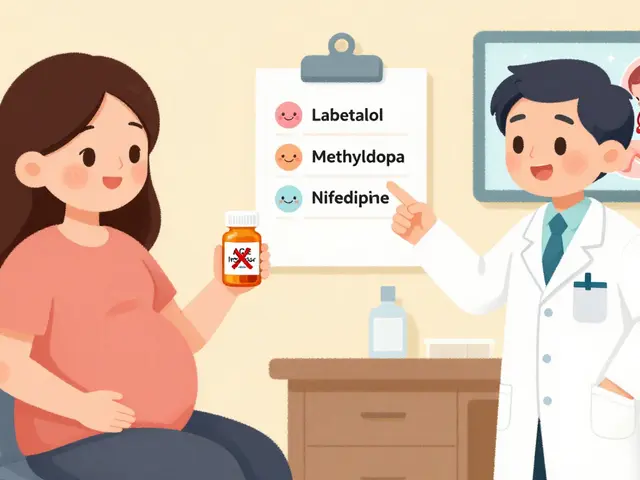
What Treatments Are Available?
If you test positive, you’re not stuck waiting it out. Antiviral pills like Paxlovid (nirmatrelvir/ritonavir) are still the gold standard for high-risk patients - people over 65, those with diabetes, heart disease, or weakened immune systems. You need to start it within five days of symptoms for it to work.
For others, it’s about managing symptoms. Rest. Hydration. Over-the-counter pain relievers. No need for antibiotics - they don’t work on viruses. If you’re struggling to breathe, or your fever won’t break after three days, call your doctor. Don’t wait until you’re gasping for air.
Monoclonal antibodies, once a go-to treatment, have mostly been phased out because they don’t work against newer variants. But one new drug, clesrovimab, got FDA approval in June 2025 - not for COVID, but for RSV in babies. It shows how much the medical world has shifted: we’re now treating multiple respiratory viruses with targeted tools, not one-size-fits-all approaches.

Why Do People Still Skip the Vaccine?
Despite all the data, 41% of unvaccinated adults in the U.S. still say they’re worried the vaccines were rushed. That’s misinformation. The science behind mRNA vaccines has been around for decades. The speed came from global funding and parallel testing - not skipped steps.
Others say, “I already had it. I’m immune.” But immunity from infection fades. And the virus keeps changing. A 2025 study in the Journal of Medical Virology found people who got infected before 2023 had little protection against XFG. The vaccine gives you a broader shield.
And then there’s the confusion. Health departments update guidelines every few months. Websites change. People don’t know what to believe. That’s why trusted sources like the CDC, Mayo Clinic, and your primary care doctor matter more than ever.
What Should You Do Now?
Here’s the simple plan for 2026:
- Get your updated 2025-2026 COVID-19 vaccine if you haven’t already. Don’t wait for symptoms.
- If you feel sick, test early. A rapid antigen test works fine at home.
- If you’re high-risk and test positive, call your doctor within 24 hours. Ask about Paxlovid.
- Wear a mask in crowded indoor spaces - especially if you’re around older people or those with chronic illness.
- Don’t panic. But don’t ignore it either. This isn’t 2020. But it’s not over.
Most people who get COVID now recover in 5 to 10 days. But for some, it lingers. The vaccine doesn’t guarantee you won’t get sick. But it gives you the best shot at not getting crushed by it.
Think of it like the flu shot. You don’t get it because you’re scared of getting the flu. You get it because you don’t want to spend a week in bed, or end up in the hospital, or pass it to your grandparent. Same logic. Same outcome.
Are the new COVID-19 vaccines safe?
Yes. The 2024-2025 and 2025-2026 vaccines use the same mRNA and protein-based technologies as earlier versions, with no new ingredients. Over 1.2 billion doses have been administered in the U.S. since 2020. Side effects are usually mild - sore arm, fatigue, headache - and fade within 48 hours. Serious reactions are extremely rare.
Can I still get COVID after being vaccinated?
Yes. The vaccines don’t block every infection, especially with new variants like XFG. But they dramatically lower your risk of severe illness, hospitalization, and death. People who are vaccinated and get infected usually have milder symptoms and recover faster. One Reddit user shared that despite catching Stratus, they were fine in three days - while their unvaccinated neighbor needed oxygen.
Do I need a vaccine if I already had COVID?
Yes. Natural immunity from past infection fades over time, and newer variants like XFG can bypass it. The CDC recommends getting the latest vaccine even if you’ve had COVID before - but wait at least three months after your symptoms started or your positive test. That gives your immune system time to recover and respond better to the vaccine.
How do I know which vaccine to get - Pfizer, Moderna, or Novavax?
All three are effective. Pfizer and Moderna target KP.2. Novavax targets JN.1 but shows strong cross-protection against other strains like KP.2 and KP.3. If you’re over 65 or have a chronic condition, talk to your doctor. Otherwise, take whichever is available first. The most important thing is getting any updated shot - not waiting for the “perfect” one.
Is long COVID still a concern in 2026?
Absolutely. About 20% of people who’ve had COVID report symptoms lasting three years or longer - fatigue, brain fog, shortness of breath, and anxiety. These aren’t rare. They’re common enough that doctors now screen for them. Getting vaccinated reduces your risk of developing long COVID by about 50%, according to a 2025 study in The Lancet. If you’re still struggling after an infection, seek help. You’re not alone.
Should I wear a mask in public now?
It depends. If you’re healthy and young, you may not need to. But if you’re around older adults, pregnant people, or those with weakened immune systems - wear one. Masks are still one of the most effective tools to reduce spread, especially in crowded indoor spaces like hospitals, buses, or airports. N95 or KN95 masks work best. Cloth masks offer little protection against today’s variants.





14 Comments
My mom got the new shot last month and she’s been fine - no side effects at all. She’s 72 and has COPD, so we were nervous, but the doctor said the benefits far outweigh any risk. Honestly, if you’re still hesitating because of 2020 fears, you’re living in the past. This isn’t the same virus anymore.
The notion that vaccines are ‘updated annually’ is a dangerous normalization of perpetual medical intervention. The human immune system evolved over millennia to handle pathogens - not to be reprogrammed every season by corporate-aligned pharmaceuticals. This is not medicine. It is managed dependency.
They’re lying about the variants. XFG? Stratus? That’s not a real name. They just made that up so you wouldn’t notice it’s the same old virus they’ve been pumping into you since 2020. The CDC doesn’t want you to know they’re just recycling old tech and calling it new. And don’t get me started on Paxlovid - it’s just a placebo with a fancy name.
I had COVID last fall and thought it was just a stubborn cold - turned out to be Stratus. Took me three weeks to feel normal again. I didn’t even realize I had brain fog until I tried to remember my own password and couldn’t. Got the new vaccine last week. Honestly? I’m not scared anymore. I just don’t want to feel like that again. It’s not about fear. It’s about not wanting to be that tired all the time.
It is imperative to underscore the significance of evidence-based public health interventions in mitigating the persistent burden of post-acute sequelae of SARS-CoV-2 infection. The epidemiological data, peer-reviewed longitudinal studies, and clinical guidelines from authoritative institutions such as the CDC and WHO provide unequivocal support for the continued administration of updated vaccines, particularly among vulnerable populations. Dissemination of misinformation undermines collective immunity and disproportionately affects marginalized communities.
If you’re not vaccinated and you’re reading this, stop. Just stop. You’re not a hero for refusing. You’re a liability. You think you’re protecting your freedom? You’re just making it harder for your neighbor, your coworker, your kid’s teacher to breathe without fear. Get the shot. It’s not a choice that affects only you.
How do we know the new vaccine actually works against XFG if it’s based on KP.2? Is there real-world data from hospitals showing lower hospitalization rates in people who got the 2025 shot versus those who didn’t? I’ve seen the lab studies but I want to know what’s happening on the ground.
Oh, please. ‘Mild side effects’? That’s what they say when they don’t want you to dig deeper. Fatigue, headache, sore arm - sure, fine. But what about the myocarditis? The Guillain-Barré? The ‘unknown long-term effects’ they conveniently ignore? You think this is science? It’s marketing dressed in lab coats. And you’re buying it.
It’s fascinating how the same people who scream ‘trust the science’ when it’s about vaccines suddenly become epistemological anarchists when it comes to mask mandates or long COVID. The cognitive dissonance is almost poetic. Or tragic. Depends on whether you’re invested in truth or just feeling superior.
They want you to take the shot because they’re scared you’ll live too long. The government doesn’t want old people around. They want the young to work and pay taxes. That’s why they push the vaccine. It’s not about health. It’s about control. And the media helps them. Don’t be fooled.
As a global health advocate with over two decades of field experience across five continents, I must emphasize the critical importance of harmonizing vaccine accessibility with cultural literacy. In many low-resource settings, misinformation is not merely a byproduct of digital platforms - it is a deliberate strategy employed by actors with vested interests in destabilizing public health infrastructure. The solution lies not in condemnation, but in community-based education, delivered with humility and respect for local epistemologies.
You think you’re smart because you got the shot? You’re just a sheep. Everyone else is waking up. They’re seeing the truth. The virus is not the enemy. The control is. The masks. The shots. The fear. They want you dependent. Don’t be their pet. Break free.
So you’re telling me I’m supposed to trust a system that got 800,000 Americans dead in 2021 and now says ‘oh by the way, here’s another shot’? I’ve seen too many people get sick after vaccines to believe this isn’t a rigged game. I’m not anti-science. I’m anti-gullibility.
Crystel Ann said her mom got the shot and was fine - that’s exactly why I got mine too. My dad’s 78 with heart disease. He didn’t want to, but after seeing how fast the new variant spreads at his senior center, he changed his mind. We’re not doing this for ourselves. We’re doing it so we don’t have to watch someone we love struggle to breathe. That’s not fear. That’s love.