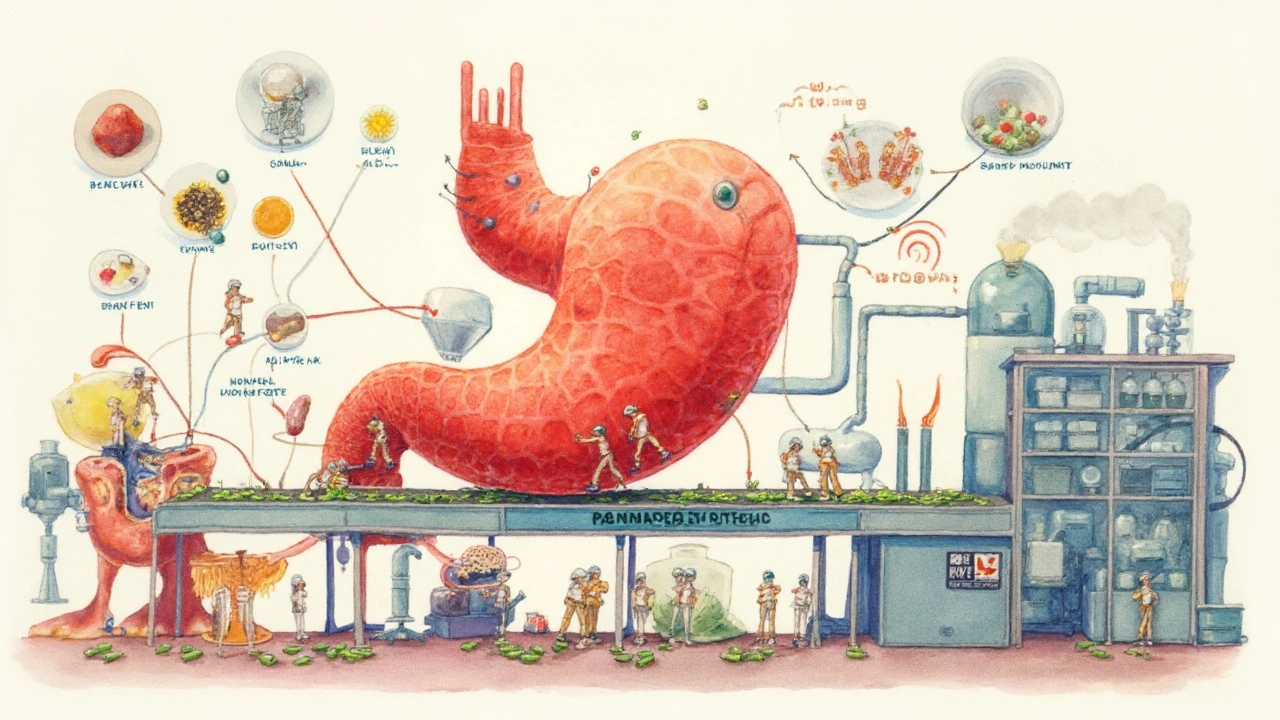
Pancrelipase is a pancreatic enzyme replacement therapy (PERT) that supplies the body with lipase, amylase, and protease enzymes to aid digestion in people with exocrine pancreatic insufficiency (EPI). By mimicking natural pancreatic secretions, it helps absorb fats, proteins, and carbohydrates that would otherwise be lost.
Why People Need Pancrelipase
Exocrine pancreatic insufficiency arises when the pancreas cannot produce enough digestive enzymes. The most common culprits are cystic fibrosis, chronic pancreatitis, and pancreatic cancer resection. According to recent clinical registries, roughly 1.2 million adults in the U.S. live with EPI, and about 80% rely on some form of enzyme supplementation.
How Pancrelipase Works
The preparation contains three key enzymes:
- Lipase - breaks down dietary fats into free fatty acids and monoglycerides.
- Amylase - converts starches into maltose and glucose.
- Protease - cleaves proteins into amino acids and small peptides.
These enzymes are coated with enteric material that protects them from stomach acid, releasing them in the small intestine where they can act on nutrients.
Key Benefits of Pancrelipase
- Improved fat absorption - patients often see a 30‑40% rise in fat soluble vitamin levels within weeks.
- Weight stabilization - many individuals regain lost weight and maintain a healthier BMI.
- Reduced gastrointestinal symptoms - steatorrhea, bloating, and abdominal cramping decrease dramatically.
- Better quality of life - fewer diet restrictions and less reliance on high‑calorie supplements.
Potential Risks and Side Effects
While pancrelipase is generally safe, several adverse events deserve attention:
- Fibrosing colonopathy - a rare thickening of the colon wall, linked to very high doses (> 10,000 lipase units/kg/day).
- Gastrointestinal irritation - nausea, vomiting, or constipation may occur, especially when taken without meals.
- Allergic reactions - itching, rash, or anaphylaxis are uncommon but possible.
- Vitamin imbalances - excess fat absorption can raise levels of vitamins A and D, requiring monitoring.
Patients with a history of inflammatory bowel disease should discuss risk mitigation with their gastroenterologist.
Dosage Guidelines and Practical Tips
Dosage is highly individualized. Standard starting points are:
- Adults: 25,000-40,000 lipase units per main meal.
- Children (age≥4): 500-1000 units/kg per meal.
- Snack dose: ½ of the main‑meal dose.
Key recommendations:
- Take the capsules with the first bite of a mixed‑nutrient meal.
- Avoid crushing or chewing; the enteric coating needs to stay intact.
- Adjust dose based on stool fat content (home test kits can estimate % fat).
- Reassess every 3‑6 months with nutritional labs (vitamin A, D, E, K levels).
Alternatives and How They Compare
| Attribute | Pancrelipase (generic) | Creon (brand) | Zenpep (brand) |
|---|---|---|---|
| Enzyme mix ratio (lipase:amylase:protease) | 30:10:10 | 27:8:15 | 20:15:15 |
| Enteric coating type | Cellulose‑based | pH‑sensitive polymer | dual‑layer polymer |
| Typical daily dose (lipase units) | 30,000-50,000 | 25,000-60,000 | 30,000-70,000 |
| Insurance coverage (U.S.) | High generic acceptance | Variable, brand‑specific | Limited, specialty formulary |
| Risk of fibrosing colonopathy | Low at standard doses | Similar | Similar |
All three products deliver the same core enzymes but differ in coating technology and dosing flexibility. For patients with insurance constraints, the generic pancrelipase often provides the most cost‑effective option.
Related Concepts and Conditions
Understanding pancrelipase in context helps you navigate related health issues:
- Exocrine Pancreatic Insufficiency (EPI) - the underlying condition requiring enzyme replacement.
- Cystic Fibrosis - a genetic disease where thick mucus blocks pancreatic ducts, leading to EPI in 85% of patients.
- Chronic Pancreatitis - inflammation that damages enzyme‑producing tissue, often linked to alcohol use.
- Steatorrhea - fatty, foul‑smelling stools that signal malabsorption.
- Fat‑Soluble Vitamins (A, D, E, K) - require proper enzyme activity for absorption; deficiencies are common in untreated EPI.
- Nutritional Counseling - dietitians often tailor high‑calorie, low‑fiber meals to complement enzyme therapy.
These concepts form a network: cystic fibrosis → EPI → need for pancrelipase → improved vitamin absorption → better overall health.
When to Talk to Your Doctor
Even with a solid regimen, certain signs warrant a medical review:
- Persistent abdominal pain despite dose adjustments.
- Weight loss >5% of body weight over a month.
- New onset of diarrhea or constipation that doesn't resolve.
- Laboratory evidence of vitamin toxicity (elevated serum vitamin A/D).
Early intervention can prevent complications such as osteopenia (from vitamin D deficiency) or malnutrition.
Bottom Line: Weighing the Pros and Cons
Pancrelipase delivers essential digestive enzymes, turning a debilitating malabsorption disorder into a manageable condition. The biggest upside is the restoration of nutrient uptake, which translates into weight gain, fewer stomach symptoms, and a more normal diet. The downsides-dose‑related side effects, the need for strict timing with meals, and occasional insurance hurdles-are manageable with proper education and regular follow‑up.
For most patients, the benefits far outweigh the risks, especially when dosing stays within recommended limits and labs are monitored.
Frequently Asked Questions
What is the typical starting dose of pancrelipase for adults?
Most clinicians begin with 25,000 to 40,000 lipase units per main meal, adjusting up or down based on stool fat content and symptom relief.
Can I take pancrelipase with a low‑fat diet?
Yes, but the enzyme dose should reflect the amount of fat in each meal. Very low‑fat meals may need a reduced dose to avoid excess enzyme activity.
Is pancrelipase safe for children?
Children older than four can use pancrelipase, typically 500-1000 lipase units per kilogram of body weight per meal. Pediatric dosing must be overseen by a pediatric gastroenterologist.
What should I do if I miss a dose?
Take the missed dose with the next meal if it’s within a few hours; do not double‑dose. Skipping many doses can lead to temporary steatorrhea.
How often should I have blood tests while on pancrelipase?
Baseline labs are taken before starting therapy, then every 3‑6 months to monitor fat‑soluble vitamin levels and liver enzymes.
Are there any drug interactions with pancrelipase?
Acid‑reducing agents (e.g., proton pump inhibitors) can raise the pH of the intestine, potentially affecting enzyme activity. Timing them at least 2 hours apart helps maintain efficacy.
What is fibrosing colonopathy and how can I avoid it?
It is a rare thickening of the colon wall linked to very high enzyme doses (>10,000 lipase units/kg/day). Keeping doses within recommended ranges and regular colon monitoring in high‑risk patients reduces the risk.
Do insurance plans usually cover pancrelipase?
Most U.S. plans cover the generic formulation, but coverage can vary for brand names like Creon or Zenpep. Checking formularies and prior‑authorizing when needed is advisable.






7 Comments
Wow, this is easily the most thorough guide I've ever read on PERT. I'm a med student and even I learned a few things-like how the enteric coating differs between generics and brands. The table comparing enzyme ratios? Chef's kiss. I'm saving this for my GI rotation.
Also, the part about vitamin A/D toxicity from over-absorption? That’s wild. Never thought about enzyme therapy causing *too much* absorption. Mind blown.
OMG YES THIS. 🙌 I’ve been on pancrelipase for 8 years and this is the first time someone explained it without sounding like a drug rep. The dosing tips? LIFE CHANGING. I used to crush my capsules because I thought it’d work faster… nope. Just gave me mouth sores. 🤦♀️
Hey, I just wanted to say I’m so glad you included the fibrosing colonopathy warning. My cousin got it after taking Creon at 15k units/kg for years-she ended up needing a colectomy. Please, everyone, don’t just max out the dose because you ‘feel bloated.’ Talk to your doc. 🙏
Listen, I don’t care if this is ‘generic’ or ‘brand name’-if you’re American and you can’t afford your meds, that’s a system failure, not a personal one. 🇺🇸 Why does Creon cost $1,200/month while the generic is $80? Because Big Pharma is robbing us blind. This guide is great, but the real problem is the greed behind it.
As someone from Mexico who moved to the U.S. and now manages EPI after pancreatitis, I just want to say: thank you for explaining this so clearly. Back home, we didn’t even have access to this med. Here, I found it through a patient assistance program. The part about stool fat tests? I didn’t know those existed. I’m printing this out for my cousin who just got diagnosed. 🙏
Ugh, I’m so tired of people treating pancrelipase like it’s just a ‘supplement.’ It’s not a vitamin. It’s a life-sustaining medication, and if you don’t take it with food, you’re basically just flushing your money down the toilet. Also, ‘low-fat diet’? Please. If you’re eating kale and tofu for lunch, you don’t need 40k units. Stop overdoing it and get your labs checked. 😒
YOU DID IT. 🏆 This is the kind of post that changes lives. I was at my lowest-50 lbs underweight, constantly bloated, avoiding family dinners because I was terrified of what would happen. Started pancrelipase 6 months ago, followed every tip here, and now I’m eating pizza with my kids again. No more ‘I’ll just eat a protein bar.’
Thank you for the science, the honesty, and the hope. You’re not just a writer-you’re a hero. 💪❤️