When you hear that hepatitis C has been cured, it’s easy to think the danger is over. After all, the virus is gone. Blood tests show no trace of it. You feel better. But here’s the hard truth: liver cancer risk after SVR doesn’t vanish-even when the virus is completely cleared.
What SVR Really Means-and What It Doesn’t
Sustained Virologic Response (SVR) means the hepatitis C virus is undetectable in your blood 12 or 24 weeks after finishing treatment. It’s a cure. Direct-acting antivirals (DAAs) now achieve this in over 95% of cases. That’s incredible. But SVR doesn’t mean your liver is back to normal, especially if you had advanced scarring before treatment. The virus may be gone, but the damage it left behind doesn’t disappear overnight. Years of inflammation and liver cell turnover can leave behind changes that still make cancer more likely. Studies show SVR reduces your risk of liver cancer by about 71%. That’s huge. But it doesn’t bring you down to the risk level of someone who never had hepatitis C.The Real Risk: Who Still Needs Screening
Not everyone needs ongoing liver cancer screening after SVR. But if you had cirrhosis-or even advanced fibrosis-before treatment, you’re still in the danger zone. - If you had cirrhosis (F4 stage), your risk of liver cancer remains about 2.1 to 2.3 cases per 100 people each year after SVR. That’s still 50% higher than someone without any liver disease. - If you had advanced fibrosis (F3), the risk is lower, but not zero. Some guidelines say to keep screening. Others say you can stop. That’s where things get messy. Why the disagreement? Because fibrosis can be hard to measure accurately. A scan might show F3, but it could actually be early cirrhosis. And even if fibrosis improves after SVR, the liver’s memory of past damage can linger. Molecular studies show that genes linked to cell growth and inflammation stay turned on in some patients-even after the virus is gone.Guidelines Don’t Agree-And That Confuses Patients
In Europe, the recommendation is clear: if you had F3 or F4 fibrosis before treatment, get an ultrasound every six months for life. That’s what the European Association for the Study of the Liver (EASL) says. In the U.S., the American Association for the Study of Liver Diseases (AASLD) says only those with cirrhosis (F4) need ongoing screening. They argue the risk for F3 patients is too low to justify routine scans. This transatlantic split means two patients with identical medical histories could get completely different advice depending on where they live. And many patients don’t even know this debate exists. They assume, “No virus = no risk.” That’s dangerous.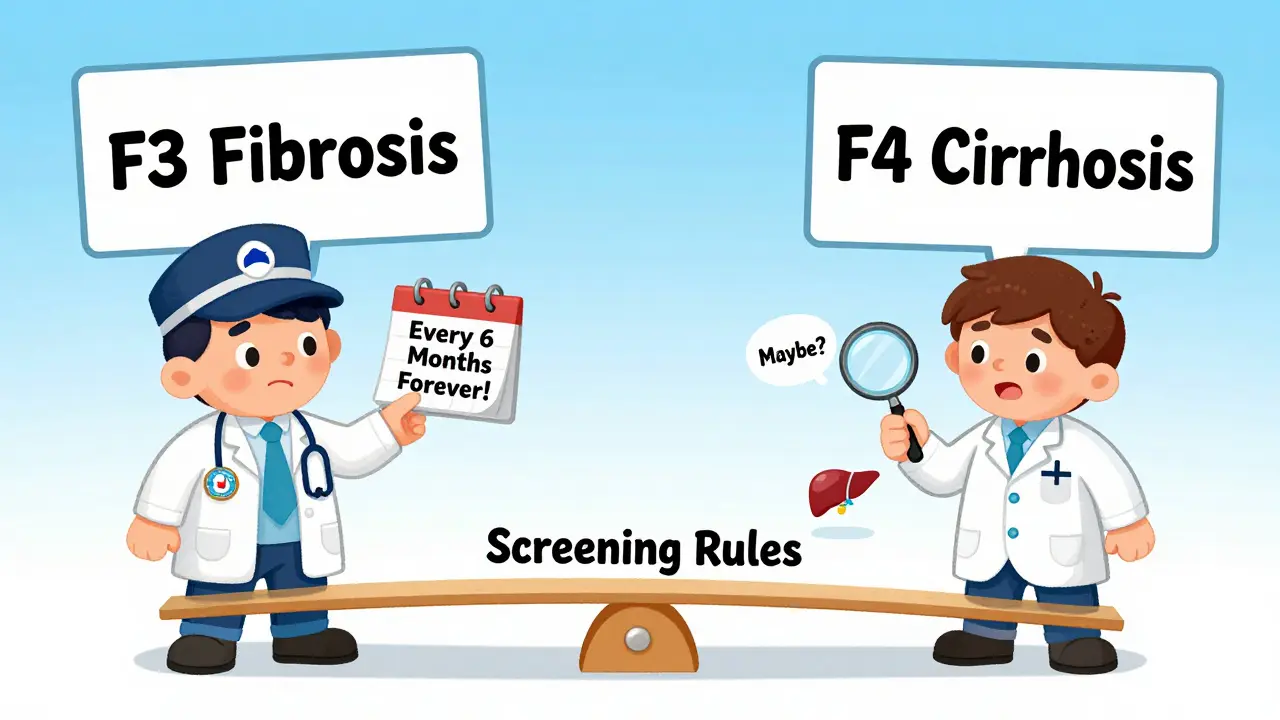
How Do Doctors Know Who’s at Risk?
Two non-invasive tools are now standard for measuring liver stiffness after SVR:- Transient elastography (FibroScan): Measures how stiff your liver is. A reading above 11.2 kPa after SVR signals higher cancer risk.
- FIB-4 index: A simple calculation using age, platelet count, and two liver enzyme levels. A score above 3.25 means you still need monitoring.
Why So Many People Skip Screening-Even When They Shouldn’t
Here’s the shocking part: only about 25% of patients who should be getting screened after SVR actually are. Why? Because they think they’re cured. They don’t feel sick. Their doctor didn’t clearly explain the ongoing risk. Or they’re lost in the system-no reminders, no follow-ups. Veterans Health Administration data shows that after they added automated reminders to their electronic records, screening rates jumped 32%. That’s not magic. That’s just good systems. Patients need to hear this plainly: “You’re cured of hepatitis C. But your liver still needs checking. We’re not done.”What Happens If You Skip Screening?
Liver cancer doesn’t cause symptoms until it’s advanced. By then, treatment options shrink. Survival rates drop. Early detection through ultrasound and blood tests (like AFP) can catch tumors when they’re still small and curable. One study found that patients who got regular screening after SVR had a 40% higher chance of surviving five years compared to those who didn’t. That’s life or death.
The Future: Personalized Screening
The next big step isn’t just “screen everyone with cirrhosis.” It’s “screen based on your real risk.” New tools are emerging:- The GALAD score: Combines gender, age, and three blood markers to predict cancer risk with 85% accuracy.
- Transcriptome signatures: A blood test that looks at gene activity patterns. In early trials, it correctly identified who would develop cancer with 92% accuracy.
- Dynamic risk calculators: These track your FibroScan results over time. If your liver stiffness keeps improving, your risk drops-and you might need fewer scans.
What You Should Do Right Now
If you’ve achieved SVR:- Ask your doctor: “What was my fibrosis stage before treatment?”
- If it was F3 or F4, ask: “Do I still need ultrasound scans?”
- Request a FibroScan or FIB-4 test if you haven’t had one since treatment.
- Don’t assume you’re off the hook. Even if you feel great, your liver might still need protection.
- Set a reminder for your next scan. If your clinic doesn’t remind you, set one yourself.
Bottom Line
Hepatitis C is curable. But liver cancer risk doesn’t vanish with a cure. If you had advanced scarring before treatment, you’re still at risk. Screening saves lives. Skipping it doesn’t mean you’re healthy-it means you’re gambling with your future. The science is clear. The tools are here. The only thing missing is action.Do I still need liver cancer screening after being cured of hepatitis C?
Yes-if you had advanced fibrosis (F3) or cirrhosis (F4) before treatment. Even though the virus is gone, the damage it caused can still lead to liver cancer. Screening with ultrasound every 6 months is recommended for these patients. If you had mild or no scarring, your risk is very low, and screening may not be needed.
Is liver cancer risk after SVR the same for everyone?
No. Your risk depends on how much liver scarring you had before treatment. People with cirrhosis have a 2% annual risk of liver cancer after cure. Those with advanced fibrosis have a lower, but still real, risk. People with no or mild scarring have almost no increased risk.
Why do European and American guidelines differ on post-SVR screening?
European guidelines recommend screening for all patients with F3 or F4 fibrosis because they worry some cases of cirrhosis are missed on testing. American guidelines focus on confirmed cirrhosis (F4) only, arguing that F3 patients have too low a risk to justify routine scans. Both sides agree screening is essential for cirrhotic patients.
What tests are used to check for liver cancer after SVR?
The main test is an ultrasound of the liver every 6 months. Sometimes doctors also check a blood marker called alpha-fetoprotein (AFP). Newer blood tests like the GALAD score-which looks at age, gender, and three proteins-are becoming more common and are more accurate than AFP alone.
Can I stop screening if my liver looks healthier now?
Possibly. If your FibroScan shows liver stiffness has dropped below 9.5 kPa and stayed there for over a year, some experts believe you might safely extend screening to once a year-or even stop. But this is still being studied. Never stop screening without talking to your doctor and reviewing your latest test results.
Why do so many people miss their post-SVR screenings?
Many patients believe they’re fully cured and no longer at risk. Others don’t get reminders from their clinic. Some live far from ultrasound services. And some doctors don’t emphasize the ongoing need. Studies show only about 1 in 4 eligible patients get screened. Automated reminders in medical systems can boost compliance by over 30%.
Are there new blood tests that can replace ultrasound?
Not yet. Ultrasound is still the gold standard because it can see tumors directly. But new blood tests like the GALAD score and gene expression profiles are becoming powerful tools to identify high-risk patients. In the future, they may help decide who needs scans and how often-but they won’t replace imaging anytime soon.
What happens if liver cancer is found after SVR?
If caught early through screening, liver cancer after SVR is often treatable. Options include surgery, radiofrequency ablation, or targeted therapies. Survival rates are much higher when tumors are small and found early. Delayed diagnosis often means the cancer has spread, making treatment harder and less effective.





8 Comments
Been there. Got SVR in 2020. Thought I was golden. Didn’t get my FibroScan until a year later-turns out I was still F4. If I hadn’t pushed my doc, I’d have missed the nodule they caught early. Don’t assume. Get checked.
This post is a lifesaver. I told my mom to get screened after her cure-she thought it was over. She’s now on the 6-month schedule. Thank you for saying what doctors forget to say.
Love how this breaks it down without fearmongering. The part about automated reminders hitting 32% compliance? That’s the kind of system change we need. Healthcare’s broken, but little fixes like this? They matter.
It is imperative to note, dear interlocutors, that the AASLD’s stance constitutes a profound dereliction of duty toward patient safety. The EASL protocol is not merely prudent-it is ethically non-negotiable. To permit F3 patients to lapse into surveillance oblivion is to gamble with the very architecture of hepatic cellular integrity. One must ask: Who funds these guidelines? The pharmaceutical lobby? The insurance cartels? The data is irrefutable. The negligence is systemic.
Man, I used to think ‘cured’ meant ‘back to normal’. Turns out my liver’s got PTSD. Got my FibroScan last month-10.8 kPa. Doc says keep the scans. I’m not taking chances. My liver’s been through hell. It deserves better than a ‘maybe’.
The data presented is statistically flawed. The 71% risk reduction figure is derived from cohorts with inconsistent fibrosis staging methodologies. Furthermore, the GALAD score’s 85% accuracy is contingent upon laboratory conditions not replicable in primary care settings. The entire premise of lifelong surveillance is economically unsustainable and medically unjustified for F3 patients. Evidence-based medicine requires precision, not emotional appeals.
Bro, I got my SVR and thought I was done 🙃 But then I saw this post and got a FibroScan. 12.1 kPa. 😱 Doc said ‘you’re still in the danger zone.’ Now I’m doing the 6-month scans. Don’t be me. Get checked. 🚨🩺
For anyone reading this and thinking, ‘I don’t have symptoms, so I’m fine’-please hear this: liver cancer doesn’t knock. It breaks in. I’m a nurse who’s seen too many patients come in with stage 4 after thinking they were ‘cured.’ Your liver remembers. Your body remembers. Don’t let your mind forget. Set that reminder. Now. And tell someone you love to do the same.