Every time you pick up your prescription, you might be getting a different pill-even if the name on the bottle hasn’t changed. That’s because most generic drugs aren’t made by one company. There are often five, ten, or even more manufacturers making the same active ingredient. And if your pharmacy or insurance switches suppliers, you could end up with a completely different-looking pill. For many people, this doesn’t matter. But for others, it can mean the difference between feeling stable and feeling worse.
Why Do Generic Switches Happen?
Generic drugs cost 80%-85% less than brand-name versions. That’s why pharmacies and insurers push them. When a drug’s patent expires, multiple companies rush to make copies. Each one has to prove it works the same way as the original. But they don’t have to prove they work the same as each other.
Insurance companies often choose the cheapest option available. Pharmacies stock whatever’s cheapest or easiest to get. If one manufacturer runs out, they switch to another. You might get Teva one month, Mylan the next, and Sandoz the month after that. None of these changes require your doctor’s approval. And most of the time, you won’t even notice-until something goes wrong.
What’s the Real Risk?
The FDA says generics must deliver between 80% and 125% of the active ingredient compared to the brand. That sounds fine-until you do the math. Two different generics could be at opposite ends of that range. One might deliver 82% of the drug. Another might deliver 123%. That’s a 41% difference in how much medicine actually gets into your body.
For most drugs, that’s not a big deal. Your body can handle small changes. But for drugs with a narrow therapeutic index-meaning the difference between a helpful dose and a dangerous one is tiny-this matters a lot.
These are the drugs where switching can cause real problems:
- Levothyroxine (for hypothyroidism): Even small changes in thyroid hormone levels can make you tired, gain weight, or feel anxious. Many patients report feeling off every time their generic changes.
- Warfarin (a blood thinner): Too little and you risk a clot. Too much and you risk bleeding. INR levels can swing after a switch, even if the dose stays the same.
- Tacrolimus (for transplant patients): A small drop in blood levels can trigger organ rejection.
- Antiepileptic drugs (like phenytoin or lamotrigine): Patients have reported breakthrough seizures after switching manufacturers.
A 2023 study found that 44% of people on antiepileptic drugs switched back to their original generic-or even the brand-because they felt worse. For thyroid meds, it was 33%. For statins? Only 8%. The risk isn’t the same across the board.
What Patients Are Saying
Online forums are full of stories like this:
"My seizure meds switched from Mylan to Teva. Two weeks later, I had two seizures. My neurologist checked my blood levels-they dropped 30%. They had to raise my dose, but I still feel off." - Reddit user, r/pharmacy, March 2024
"Every time my levothyroxine changes, my TSH goes haywire. I feel like I’m getting sick for weeks. My doctor says it’s the generic. I’ve stopped letting them switch me unless I have no choice." - Drugs.com patient, May 2024
But not everyone has problems. Many people take generic lisinopril, metformin, or atorvastatin for years and never notice a difference. One GoodRx user wrote: "I’ve had five different generic manufacturers for my blood pressure pill. My numbers are perfect every time."
So why the difference? It comes down to the drug-and the person.
How to Protect Yourself
If you’re on a high-risk medication, don’t wait for a problem to happen. Take action now:
- Check your pills. Look at the shape, color, and imprint code every time you get a refill. If it looks different, ask the pharmacist: "Is this the same manufacturer as last time?"
- Ask your doctor to write "Dispense as Written" or "Do Not Substitute" on your prescription. This legally prevents the pharmacy from switching your generic without approval.
- Request a specific generic manufacturer. If you’ve had good results with Teva or Mylan, ask your doctor to specify it on the script. Pharmacies can usually honor this, especially if you explain it’s for stability.
- Get blood tests after a switch. If you’re on warfarin, levothyroxine, or tacrolimus, ask for a follow-up test 2-4 weeks after a manufacturer change. Don’t assume your dose still fits.
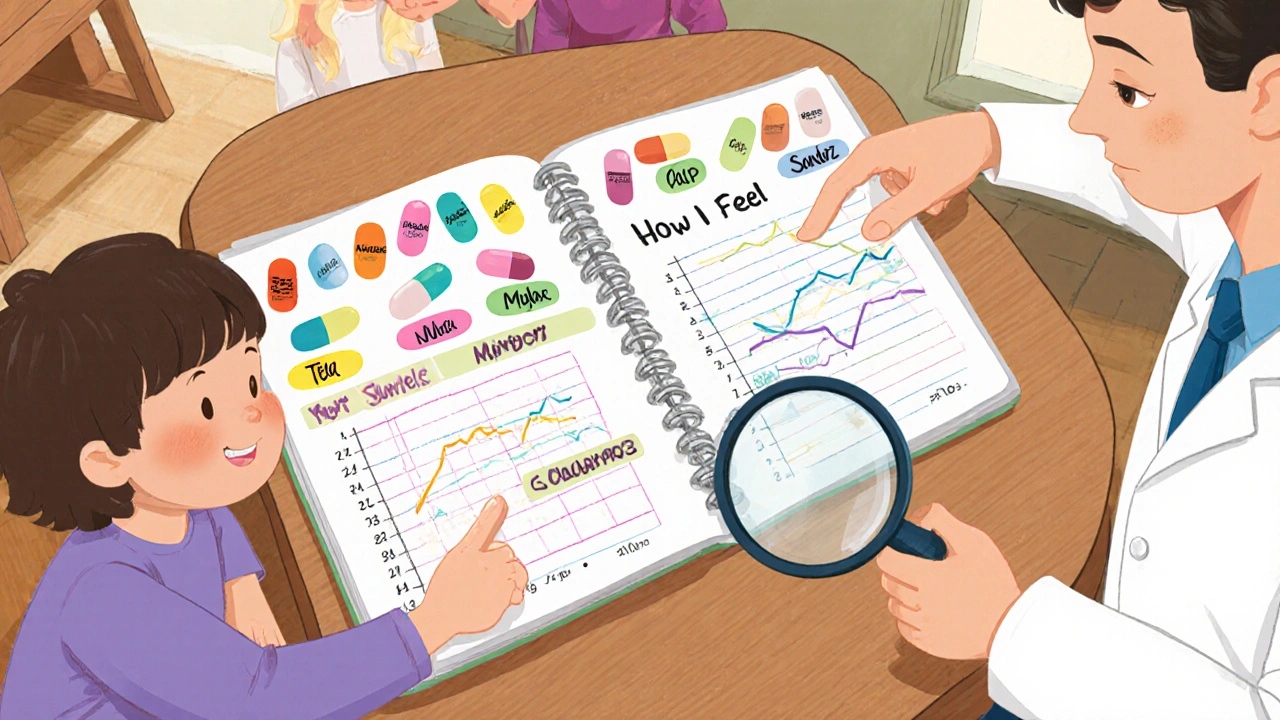
- Keep a medication log. Write down the name, manufacturer, and how you feel each time you refill. This helps your doctor spot patterns.
Some hospitals and clinics now use "lock-in" programs for NTI drugs. Once you’re on a specific generic, you stay on it unless something changes medically. That’s the gold standard-and it’s becoming more common.
What’s Being Done?
Regulators are starting to pay attention. In June 2024, Medsafe (New Zealand’s drug agency) advised doctors to avoid switching levothyroxine brands unless absolutely necessary. The FDA launched a pilot program in 2023 requiring generic makers to report major formulation changes. They’re also working on better ways to test if one generic can safely replace another.
The Generic Pharmaceutical Association is working on a standardized pill ID system. Right now, the same drug can look completely different depending on who made it. Imagine if every insulin pen looked different every time you got a refill. That’s what’s happening with many generics.
But until those changes roll out, the responsibility falls on you and your doctor.

When Switching Is Fine
Not all generics are risky. For drugs like ibuprofen, simvastatin, or metformin, switching between manufacturers rarely causes issues. Your body can handle the small variations. If you’re not having side effects and your condition is stable, there’s no need to fight every switch.
The key is knowing which drugs need extra care. If you’re unsure, ask your pharmacist: "Is this a narrow therapeutic index drug?" They’re trained to know.
Bottom Line
Generic drugs save billions every year. That’s a good thing. But assuming all generics are identical is dangerous. For some medications, even small changes can have big consequences.
You don’t have to avoid generics. But you do need to be smart about them. Know your drug. Know your manufacturer. Know your symptoms. And don’t be afraid to speak up if something feels off. Your health isn’t a cost-saving experiment.
Can I ask my pharmacy to always give me the same generic manufacturer?
Yes. You can ask your pharmacist to fill your prescription with a specific generic brand. Some pharmacies will do it without a doctor’s note, especially if you’ve had problems before. If they say no, ask your doctor to write "Dispense as Written" on the prescription. This legally stops automatic substitutions.
Why do generic pills look different every time?
Generic manufacturers aren’t required to match the appearance of the brand or other generics. They can change the color, shape, or imprint to distinguish their product. That’s why you might get a blue oval one month and a white capsule the next-even if it’s the same drug. Always check the imprint code (the letters/numbers on the pill) to confirm it’s the right medication.
Is it safe to switch between generics for blood pressure or cholesterol meds?
For most people, yes. Drugs like lisinopril, atorvastatin, and metoprolol have wide therapeutic windows, meaning small changes in blood levels don’t cause major problems. Studies show fewer than 10% of patients report issues after switching these generics. But if you notice new side effects-dizziness, fatigue, or unusual swelling-tell your doctor. Don’t assume it’s "just the generic."
What should I do if I think a generic switch caused my symptoms?
First, check your pill against your last refill. If the manufacturer changed, note the name. Then contact your doctor and pharmacist. Ask for a blood test if you’re on a narrow therapeutic index drug (like warfarin or levothyroxine). Keep a log of your symptoms and when they started. Many doctors will switch you back to your original generic if they see a clear pattern.
Are brand-name drugs better than generics?
For most people, no. Generics have the same active ingredient and meet the same FDA standards. The difference isn’t quality-it’s consistency. Some people do better on one generic than another, not because it’s "better," but because their body responds differently to small changes in inactive ingredients or how the drug is absorbed. If you’re stable on a generic, stick with it. If you’re not, ask why.
Can insurance force me to switch generics?
Yes, unless your doctor has written "Do Not Substitute." Insurance companies often change which generics they cover to save money. They don’t have to tell you. That’s why it’s important to check your pills at the pharmacy and ask questions. If you’re on a high-risk drug, ask your doctor to request a prior authorization for a specific generic-this can prevent automatic switches.
How often should I get blood tests after a generic switch?
For narrow therapeutic index drugs like warfarin, levothyroxine, or tacrolimus, get a blood test 2-4 weeks after any manufacturer change. For warfarin, that means an INR test. For thyroid meds, it’s TSH and free T4. Waiting longer than a month risks missing a dangerous shift. Don’t wait for symptoms-test early.




12 Comments
The variability in generic drug formulations is a systemic issue that deserves regulatory attention. The FDA's 80%-125% bioequivalence window is statistically acceptable for population-level outcomes but ignores individual pharmacokinetic variance. For patients on narrow therapeutic index drugs, this isn't just a clinical concern-it's a matter of physiological stability. The lack of mandatory manufacturer consistency protocols is indefensible when lives are at stake.
lol so now even pills have identity crises 🤡
You people treat pharmaceuticals like groceries. The entire system is a grotesque commodification of human biology. A pill isn't a commodity-it's a molecular covenant between chemistry and physiology. When you reduce life-sustaining medication to a bidding war between conglomerates, you're not saving money-you're gambling with neurochemistry. This isn't capitalism. It's pharmacological nihilism.
i been on generic lisinopril for 7 years and never had an issue my bp is perfect so stop freakin out everyone dont need to panic over every pill change
Of course you’re fine on lisinopril-you’re not on levothyroxine, warfarin, or tacrolimus. The fact that you equate stability across all generics reveals a dangerous lack of nuance. Some drugs are like tuning a Stradivarius; others are like tuning a ukulele. One size does NOT fit all. And your cavalier attitude is exactly why people end up in the ER.
My neurologist told me to stop letting them switch my lamotrigine after I had three seizures in six weeks. One month it was Mylan-purple oval. Next month Teva-white capsule. Blood levels dropped 38%. I had to beg for the original. Now I pay out of pocket. They call it "cost-saving." I call it medical malpractice by spreadsheet. My body isn’t a budget line item. And if you think it is, you haven’t felt a seizure.
It is not merely a matter of pharmaceutical equivalence; it is a profound epistemological failure of modern healthcare systems. We have outsourced the sanctity of therapeutic consistency to corporate logistics, where profit margins dictate molecular fidelity. The patient becomes a variable in an algorithm, not a subject of care. This is not innovation. It is dehumanization dressed in the garb of efficiency. The pill that saves your life should not be subject to supply chain whims.
Look, I’m a pharmacist in Mumbai and I’ve seen this play out for 15 years. For statins? No problem. For levothyroxine? Absolute chaos. Patients come back crying because their TSH jumped from 2.1 to 9.8 after a switch. We keep a log of manufacturers here-same as the hospital in Delhi. If you’re on a high-risk med, always ask for the brand name on the blister pack. And if they say no, tell them you’ll go to another pharmacy. They’ll bend. It’s not about being difficult-it’s about not dying.
They’re testing us. The pharma-industrial complex is using generics as a behavioral control tool. The different colors, shapes, and imprints? That’s deliberate. They want you to feel disoriented. Confused patients don’t question. They just take the pill. And when you get sick? It’s "your body’s fault." They’ve been doing this since the 80s. The FDA? Complicit. Insurance? Enablers. Your doctor? Probably told you to shut up and take it. Wake up. This isn’t medicine. It’s psychological manipulation disguised as cost-efficiency. 🕵️♀️💊👁️
Let me be brutally honest: if you can’t handle a pill changing color, you shouldn’t be on a chronic med. Life doesn’t come with a consistent manufacturer. Your thyroid doesn’t care if Teva or Mylan made it. You’re just emotionally attached to the shape of your medicine. Get over it. The real problem? You’re addicted to control, not the drug. The system works. You’re just too fragile to adapt.
Hi everyone-I’ve been on levothyroxine for 12 years and switched manufacturers 17 times. I kept a spreadsheet: date, manufacturer, TSH, symptoms, sleep quality, mood. After 3 switches, I noticed a pattern: whenever it was Teva, I gained 4 lbs and felt foggy for 3 weeks. My doctor finally wrote "Dispense as Written" for Mylan. Now I’m stable. It took me 10 years and a spreadsheet, but I learned: your body keeps score. Write it down. Talk to your pharmacist. Ask for the pill imprint. You’re not being paranoid-you’re being proactive. And if your doctor rolls their eyes? Find a new one. You deserve consistency. 💪📊❤️
You got this. Speak up. Demand the same maker. Get the test. Keep a log. Your health is worth fighting for. No one else will do it for you.