Asthma vs Anxiety Symptom Checker
This tool helps determine if your breathing difficulties may be due to asthma, anxiety, or a combination of both. Answer the following questions honestly to get insights into possible causes.
1. Do you experience shortness of breath that occurs mainly during stress or panic attacks?
2. Do you have chest tightness that feels like pressure or a "butterfly" sensation?
3. Are you using a rescue inhaler more than twice a day?
4. Do you feel intense fear or dread when experiencing breathlessness?
5. Is your breathing difficulty worse at night or during rest?
When breathing feels like a battle, the mind often jumps in, turning a physical flare‑up into a mental tug‑of‑war. Bronchial asthma is a chronic inflammatory disease of the airways that causes episodes of wheezing, shortness of breath, and chest tightness. It affects roughly 300 million people worldwide and is driven by a hyper‑responsive immune system, excessive mucus, and bronchoconstriction. Anxiety disorders are a group of mental health conditions characterized by excessive, persistent worry, fear, or nervousness that interferes with daily life. The two conditions often appear together, creating a loop where breathing trouble fuels worry, and worry makes breathing worse. Understanding that loop is the first step toward breaking it.
Quick Takeaways
- Inflammatory cytokines released during asthma attacks can trigger the brain’s stress response.
- Symptoms like shortness of breath and chest tightness are common to both asthma and anxiety, leading to misinterpretation.
- High cortisol levels from chronic anxiety can worsen airway inflammation.
- Integrated treatment-combining inhaled medication with psychotherapy-improves control for most patients.
- Seek professional help if you notice a sudden rise in asthma attacks after a stressful event.
Why the Body Links Asthma and Anxiety
Two biological systems talk to each other more than you might think: the immune system and the nervous system. When an asthma trigger (like pollen or cold air) hits, immune cells release inflammatory cytokines proteins such as interleukin‑5 and tumor‑necrosis factor‑α that cause airway swelling and mucus production.. These same cytokines can cross the blood‑brain barrier and activate the hypothalamic‑pituitary‑adrenal (HPA axis the body’s central stress‑regulation system.), prompting the release of cortisol the primary stress hormone.. Elevated cortisol, in turn, heightens the brain’s alarm system, making a person more prone to panic and worry.
On the flip side, chronic anxiety keeps the HPA axis turned on, flooding the body with cortisol and adrenaline. These hormones can increase airway smooth‑muscle tone, making the bronchi more prone to constriction during an asthma trigger. In short, a vicious cycle forms: inflammation fuels stress, and stress fuels inflammation.
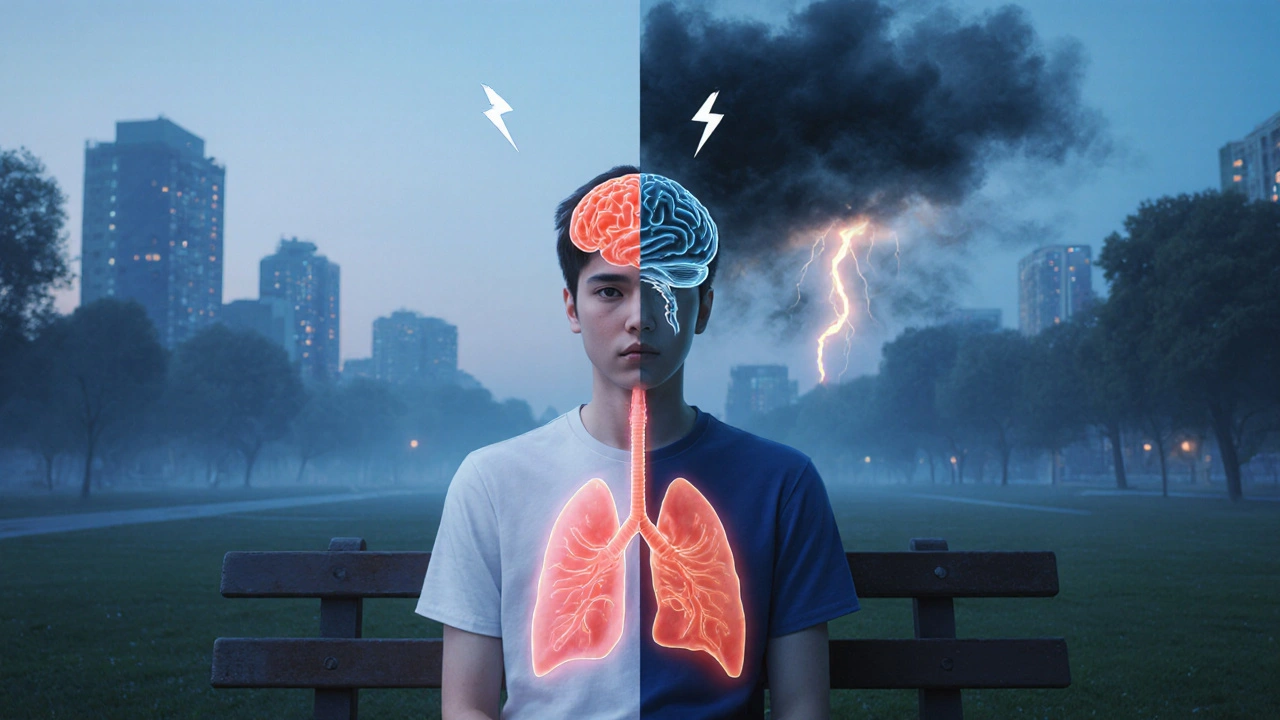
Shared Symptoms: When Breathlessness Isn’t Just Asthma
Both conditions can manifest with similar physical cues, which is why patients often mistake anxiety spikes for asthma attacks and vice‑versa. Below is a side‑by‑side look at the most common overlapping symptoms.
| Bronchial Asthma | Anxiety Disorder |
|---|---|
| Shortness of breath | Feeling of breathlessness or “air hunger” |
| Chest tightness | Chest pressure, “butterfly” feeling |
| Rapid breathing (tachypnea) | Hyperventilation |
| Feelings of dread during an attack | Intense fear or panic during episodes |
| Cough, especially at night | Cough from throat clearing due to anxiety‑induced dryness |
Because the overlap is so strong, clinicians recommend keeping a symptom diary that notes triggers, medication use, and emotional state. This data helps separate pure asthma flare‑ups from anxiety‑driven sensations.
How Anxiety Impacts Asthma Control
Research from the American Thoracic Society (2023) shows that patients with comorbid anxiety experience 30‑40% more emergency department visits for asthma than those without anxiety. Several mechanisms explain this trend:
- Medication adherence drops: Worry about side effects or fatalism can lead to missed inhaler doses.
- Altered breathing patterns: Shallow, rapid breaths increase airway resistance and can trigger bronchospasm.
- Exacerbated inflammation: Chronic cortisol spikes amplify cytokine release, worsening airway edema.
- Increased perception of symptoms: Heightened body awareness makes mild airway narrowing feel catastrophic.
These factors collectively reduce the effectiveness of standard asthma therapy and raise the risk of long‑term lung function decline.
Integrated Management Strategies
Breaking the cycle requires a two‑pronged approach: treat the lungs and calm the mind.
1. Optimize Asthma Medication
- Use inhaled corticosteroids (ICS) the gold‑standard anti‑inflammatory therapy for persistent asthma. Ensure proper inhaler technique; a spacer can improve drug delivery.
- Consider a long‑acting beta‑agonist (LABA) for patients whose symptoms aren’t controlled with ICS alone. Only use LABA in combination with an inhaled steroid.
- Monitor peak flow daily during stressful periods to catch early declines.
2. Address the Psychological Side
- Cognitive‑Behavioral Therapy (CBT): Proven to reduce anxiety scores by up to 25% in asthma patients (JACI, 2022).
- Mindful breathing exercises: Techniques such as the 4‑7‑8 breath can reset the autonomic balance, reducing airway reactivity.
- Relaxation training: Progressive muscle relaxation before bedtime cuts nocturnal cough episodes.
- Medication: Selective serotonin reuptake inhibitors (SSRIs) may be prescribed when anxiety is moderate to severe, but always coordinate with the asthma specialist to avoid drug interactions.
3. Lifestyle Tweaks
- Regular aerobic activity (e.g., brisk walking) improves lung capacity and releases endorphins that lower anxiety.
- Maintain a low‑sodium, anti‑oxidant‑rich diet; omega‑3 fatty acids have modest anti‑inflammatory effects.
- Avoid caffeine and nicotine, both of which can trigger anxiety spikes and airway irritation.
Putting these pieces together often requires a care team that includes a pulmonologist, a mental‑health professional, and a primary‑care physician. Communication among them ensures that medication schedules, therapy appointments, and lifestyle recommendations don’t clash.
When to Seek Professional Help
If you notice any of the following, it’s time to call your doctor:
- More than two rescue‑inhaler uses in a day, especially after a stressful event.
- Persistent nighttime awakenings due to coughing or panic.
- Feeling out of control with worry that interferes with work, school, or relationships.
- Signs of depression, such as loss of interest or hopelessness, appearing alongside asthma flare‑ups.
Early intervention can prevent the progression to severe asthma or chronic anxiety, both of which carry long‑term health costs.
Frequently Asked Questions
Can anxiety cause an asthma attack?
Yes. Anxiety spikes cortisol and adrenaline, which can tighten airway muscles and amplify inflammation, making an attack more likely.
Do inhaled steroids affect mood?
Inhaled steroids act locally in the lungs and have minimal systemic absorption, so they rarely influence mood. Oral steroids, however, can cause irritability or anxiety.
Is CBT covered by insurance for asthma patients?
Many plans cover CBT when it’s prescribed for a diagnosed anxiety disorder, even if the primary reason is asthma‑related stress. Always check your provider’s mental‑health benefits.
How can I tell if my shortness of breath is asthma or anxiety?
Keep a diary. Note the trigger (allergen, exercise, stressful meeting), time of day, response to rescue inhaler, and any accompanying thoughts. A pattern where anxiety precedes breathing difficulty often points to a psychogenic component.
What lifestyle changes help both conditions?
Regular aerobic exercise, a balanced anti‑inflammatory diet, good sleep hygiene, and stress‑reduction practices like yoga or tai chi benefit lung function and emotional balance.





20 Comments
Honestly, this article reads like a high‑school science project that somehow got a fancy layout. The so‑called “integrated treatment” feels like buzzword bingo rather than real guidance.
Reading through the overview of how asthma and anxiety interrelate sparked a lot of thoughts. First, the biological loop involving cytokines and the HPA axis is described with sufficient detail to be useful for clinicians. It is noteworthy that interleukin‑5 and TNF‑α can cross the blood‑brain barrier and potentially amplify stress responses. The article also mentions cortisol’s role in increasing airway smooth‑muscle tone, which aligns with recent immunology findings. I appreciate the inclusion of a symptom diary as a practical tool-patients often underestimate the value of tracking emotional states alongside physical triggers. The suggestion to monitor peak flow during stressful periods is something I have seen work in my own practice. Moreover, the emphasis on cognitive‑behavioral therapy echoes the growing body of evidence that CBT can reduce inhaler use by up to a quarter. The description of mindful breathing exercises, such as the 4‑7‑8 technique, provides a concrete strategy that patients can start immediately. While the piece outlines pharmacologic options, it wisely cautions about systemic steroid side effects on mood. The diet recommendations, especially omega-3 intake, are a nice touch but could have benefited from more specific food examples. I would have liked to see a brief discussion on the potential interactions between SSRIs and certain bronchodilators. The reference to the 2023 American Thoracic Society study adds credibility, although a direct link would have been helpful. Overall, the article balances medical facts with actionable advice without descending into jargon overload. It respects readers who may be new to the topic while still offering depth for professionals. Finally, the FAQ section anticipates common concerns and provides concise answers, making the whole piece feel complete.
Hey everyone! This guide really shines a light on how tightly our lungs and minds are linked 😊. If you’re battling both asthma and anxiety, you’re not alone, and the combined approach here is exactly what many of us need. Keep sharing your experiences and remember that small steps-like a five‑minute breathing exercise each morning-can make a big difference.
Oh great, another list of “quick takeaways” that sounds like it was copy‑pasted from a self‑help brochure. As if a lavender‑scented inhaler will magically quiet your inner drama queen. Sure, sprinkle some yoga on it and hope for the best.
I get how overwhelming it can feel when breathlessness and worry collide it’s like two rooms fighting for the same space I’m here to remind you that tracking triggers can help you find a pattern and maybe take some of the anxiety out of the equation
Wow!!! You really think this article is nothing but “buzzword bingo”???!! Let’s pause and consider that the very act of labeling complex physiological‑psychological interactions is itself a philosophical breakthrough!! Dismissing it as frivolous undermines the lived reality of countless patients!!!
Fantastic analysis!!! Your thorough breakdown really captures the nuance of the immune‑stress feedback loop 😮. I especially love the point about symptom diaries-they’re the unsung heroes of personalized medicine!!!
Sure, but have you ever wondered why the pharma industry pushes inhalers while quietly funding “mind‑set” programs? It’s like they want us to think the solution is in our heads while they profit from our panic attacks. Just a thought.
Totally agree, it’s spot on!
Let’s be clear: the Western medical narrative glorifies “integrated care” while ignoring traditional healing practices that have kept our ancestors breathing for centuries. The over‑reliance on steroids is a cultural colonization of our lungs, and we must reject it.
While the previous post glorifies “integrated care,” it conveniently omits the fact that many of these studies suffer from methodological flaws. Moreover, the article’s claim that CBT reduces inhaler usage by “up to a quarter” is misleading without proper statistical context.
Let’s keep the momentum going! 🚀 Remember, consistency in both medication adherence and mental‑health exercises can turn the tide on symptoms. You’ve got this-keep pushing forward!
It’s interesting to see how different cultures approach the asthma‑anxiety link. In some Asian traditions, breathing exercises are a core part of daily life, which may naturally mitigate anxiety‑driven bronchoconstriction. Cross‑cultural exchange could enrich treatment protocols worldwide.
From a pulmonology standpoint, the article correctly emphasizes the role of inhaled corticosteroids (ICS) as the cornerstone of persistent asthma management. However, the discussion could benefit from clarifying the distinction between adherence‑related pharmacokinetics and pharmacodynamics.
People need to stop using excues like “stress” to avoid taking responsibility for their health. If you keep making up an excuse, you’ll never improve.
Whoa there!!! Let’s not pretend that a simple diary will magically solve the complex biopsychosocial nightmare you’re describing!!! While I applaud the intention behind “track your triggers,” the reality is that many patients lack the cognitive bandwidth to maintain such records consistently!!! Moreover, the suggestion that “mindful breathing” can offset cortisol surges is, frankly, overly optimistic!!! We need robust, evidence‑based interventions, not just feel‑good pep talks!!!
That’s a solid overview. Good points all around.
Wow, the passion in that post is electrifying! While I respect the call to honor traditional practices, let’s not forget that modern medicine has saved countless lives. Balance is key, darling.
Honestly, everyone’s making a fuss over a few breathing exercises. The real problem is people don’t follow the basic advice: take meds, avoid triggers, and quit overthinking.
In the context of global health, integrating psychoneuroimmunology insights with community‑based respiratory programs could foster more resilient healthcare models, especially in low‑resource settings where stigma around mental health remains a barrier.