Nose Blockage & Eye Redness Symptom Checker
Potential Cause Analysis
Home Remedies
Try saline rinses, humidifiers, and avoiding triggers to ease symptoms.
When to See a Doctor
Seek medical attention if symptoms persist beyond a week or include severe pain.
When you wake up with a blocked-up nose and your eyes are red and watery, it’s a sign that something in your airway or eye surface is irritated. Most of the time the problem isn’t serious, but figuring out why it’s happening can save you from unnecessary discomfort and help you avoid future flare‑ups.
What is nasal congestion?
Nasal congestion is a condition where the nasal passages become swollen and filled with mucus, making it hard to breathe through the nose. The swelling is usually caused by blood vessels expanding in response to inflammation. When the airflow is blocked, you often feel pressure around the forehead and cheeks, and the excess mucus can drip down the back of the throat.
Common causes of a blocked‑up nose and red, watery eyes
Several triggers can set off the same chain reaction in the nose and eyes. Below are the most frequent culprits.
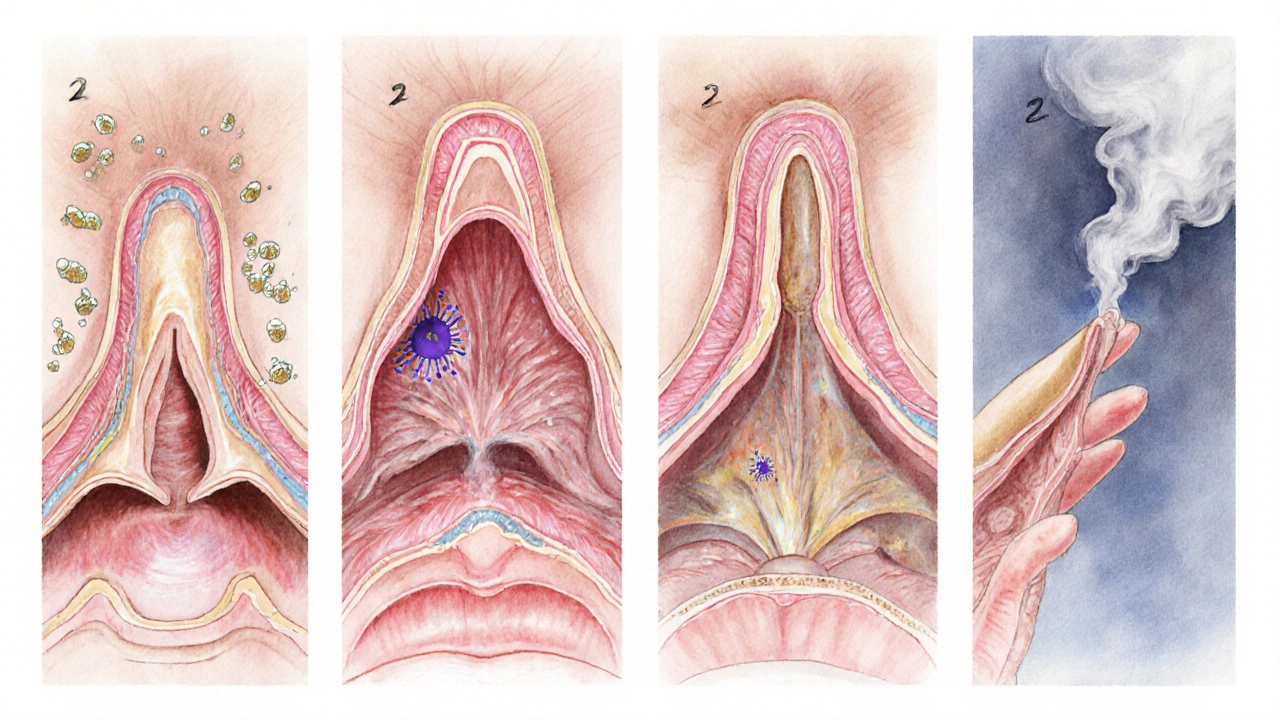
Allergic rhinitis
Allergic rhinitis is an immune‑mediated response to airborne allergens such as pollen, dust mites, pet dander or mold spores. When you inhale the allergen, your body releases histamine, a chemical that makes the blood vessels in the nose widen and the lining swell. The same histamine reaches the eyes, causing the tiny blood vessels on the surface to expand, which makes them look red and leads to excess tearing.
Viral infection (common cold)
The common cold is caused by a variety of viruses, most often rhinoviruses. These viruses infect the lining of the nasal passages and throat, prompting the body to produce mucus to trap and flush the invaders. The inflammation also irritates the nearby tear ducts, so the eyes become watery and sometimes pink.
Sinusitis
Sinusitis is an inflammation of the sinus cavities, either from a lingering infection or from swelling that blocks normal drainage. When the sinuses can’t drain, mucus backs up into the nose, worsening congestion. Pressure from the blocked sinuses often pushes fluid toward the eyes, adding to the redness and tearing.
Irritant rhinitis
Exposure to smoke, strong perfumes, chemical fumes, or sudden temperature changes can trigger irritant rhinitis, a non‑allergic inflammation of the nasal mucosa. The response is similar to allergy‑driven swelling but without the immune‑system involvement. Irritants also stimulate the eyes directly, leading to a gritty, watery feeling.
COVID‑19
Although many people think of fever and cough with COVID‑19, the virus can also cause nasal blockage and conjunctival irritation. The virus attacks the cells lining both the nose and the eyes, so a sudden onset of a blocked‑up nose paired with red eyes should prompt a rapid test, especially if you’ve been exposed.
Why do the eyes turn red and watery?
The eyes and nose are connected by the nasolacrimal duct, a tiny channel that drains tears from the eye surface into the nasal cavity. When the nasal lining swells, the duct can become partially blocked, causing tears to pool on the eye surface. At the same time, inflammation releases histamine and other mediators that dilate the tiny vessels on the eye’s surface, giving that red appearance.
How to tell if you need medical help
- Fever above 38°C (100.4°F) that lasts more than 48hours.
- Severe facial pain or swelling that worsens rather than improves.
- Green or yellow mucus that persists for more than a week.
- Sudden loss of smell or taste, especially if you suspect COVID‑19.
- Eye pain, visual changes, or light sensitivity.
If any of these red flags appear, schedule a visit with your GP or an urgent care clinic.
Quick relief tips you can try at home
- Use a saline nasal rinse to flush out mucus and allergens. Warm saline (about 0.9% salt) poured through a neti pot or squeeze bottle can clear the passages within minutes.
- Apply a cool compress over closed eyes for 5‑10minutes to shrink blood vessels and reduce redness.
- Take an over‑the‑counter antihistamine if you suspect an allergic trigger. Second‑generation options like cetirizine work without the heavy drowsiness.
- Run a humidifier in your bedroom at night to keep nasal membranes moist.
- Avoid known irritants - smoke, strong fragrances, and sudden temperature shifts - until symptoms subside.

Comparison of the most common causes
| Cause | Typical trigger | Duration | Accompanying symptoms | First‑line treatment |
|---|---|---|---|---|
| Allergic rhinitis | Pollen, dust mites, pet dander | Weeks to months (seasonal or perennial) | Sneezing, itchy throat, clear watery mucus | Antihistamines, nasal steroid spray, avoidance |
| Common cold | Rhinovirus, coronavirus (non‑COVID) | 5‑10days | Sore throat, mild fever, productive mucus | Rest, hydration, saline rinse, decongestant if needed |
| Sinusitis | Prolonged infection or blockage | 2weeks or more (acute vs chronic) | Facial pressure, thick yellow mucus, reduced smell | Saline rinse, nasal steroid, antibiotics if bacterial |
| Irritant rhinitis | Smoke, fumes, strong odors, temperature changes | Hours to a few days after exposure | Burning sensation, dry cough, non‑allergic itching | Avoid irritant, humidify air, saline rinse |
Preventing future episodes
- Keep windows closed on high‑pollen days and use HEPA filters.
- Wash bedding weekly in hot water to kill dust mites.
- Stay hydrated; thin mucus drains more easily.
- Maintain indoor humidity between 30‑50% to prevent drying of nasal lining.
- Consider a short course of nasal steroids in the spring if you have chronic seasonal allergies.
Frequently Asked Questions
Can a cold cause eye redness?
Yes. A viral cold inflames the nasal lining, and the nearby tear ducts often become irritated, leading to red, watery eyes. The condition usually clears up as the cold resolves.
Why does my nose stay blocked after I stop taking allergy meds?
When you stop antihistamines, the body’s histamine response can rebound if the underlying allergen is still present. Continuing a nasal steroid spray can keep inflammation down while you work on allergen avoidance.
Is a saline rinse safe for children?
Yes, as long as the water is sterile or boiled and cooled, and the salt concentration matches normal saline (0.9%). Use a child‑friendly squeeze bottle and supervise the process.
When should I suspect COVID‑19 instead of a regular cold?
If you have a sudden loss of taste or smell, a fever over 38°C, or have been in close contact with a confirmed case, take a rapid antigen test. COVID‑19 can present with both nasal blockage and red eyes, so testing is the safest move.
Can dehydration make my nose feel more blocked?
Absolutely. When you’re dehydrated, the mucus becomes thicker and sticks to the nasal walls, making airflow harder. Drinking plenty of water and using a humidifier can thin the mucus and relieve pressure.






15 Comments
We can't ignore how Indian cities spew pollen‑laden smog that clogs our noses and reddens our eyes, a daily reminder that the government’s lax policies are a major culprit. When you step outside during the monsoon, those microscopic dust particles hitch a ride on the humidity and strike instantly. If you want relief, the only real fix is stricter emission controls and better public awareness about indoor air filters. Until then, a saline rinse and staying indoors during peak traffic hours are the best you can do.
Honestly, it’s pretty obvious – allergies are the most common reason for that stuffy nose and red eyes. Just keep your windows closed when pollen counts are high and you’ll feel better.
Wow!!! The connection between the nasolacrimal duct and congestion is fascinating!!! Keep those humidifiers running; they actually thin mucus!!!
From a pathophysiological standpoint, the mucosal edema precipitates a ventilation‑perfusion mismatch within the sinonasal cavity, thereby amplifying histaminergic responses that extend to the ocular conjunctiva. Implementing intranasal corticosteroids alongside second‑generation antihistamines can modulate the inflammatory cascade effectively.
Stay hydrated and use a neti pot – it can clear out allergens fast.
Great, another post telling us to drink water and use saline. Because that’s never been said before.
Dear readers, allow me to elucidate the intricate ballet of mucosal inflammation that governs our nasal passages.
When airborne irritants penetrate the delicate epithelium, a cascade of cytokines is unleashed, orchestrating vasodilation and goblet cell hyperactivity.
The resultant edema not only impedes airflow but also exerts pressure upon the nasolacrimal duct, culminating in ocular hyperemia.
One must appreciate that this physiological symphony is not merely a nuisance but a testament to the body's vigilant defense mechanisms.
Yet, in our modern epoch, the prevalence of particulate matter and synthetic fragrances has amplified these responses beyond their evolutionary design.
Consequently, the average individual now endures chronic congestion and persistent ocular redness, conditions once reserved for seasonal afflictions.
It is incumbent upon us, therefore, to adopt both prophylactic and therapeutic stratagems.
Prophylaxis begins with environmental stewardship: minimizing indoor dust accumulation, employing HEPA filtration, and curbing incense combustion.
Therapeutically, isotonic saline irrigation offers immediate mechanical clearance of particulate load.
Adjunctive pharmacotherapy with intranasal corticosteroids attenuates the inflammatory surge without precipitating systemic side effects.
Antihistamines, particularly the second‑generation agents, mitigate histamine‑mediated vasodilation, thereby reducing both nasal swelling and conjunctival erythema.
Moreover, humidification of ambient air restores mucosal hydration, fostering optimal ciliary function.
In cases where bacterial superinfection ensues, a judicious course of antibiotics may be warranted, though overprescription remains a pervasive concern.
Patients should remain vigilant for red‑flag symptoms such as high fever, unilateral facial pain, or visual disturbances, which warrant immediate medical evaluation.
Ultimately, the confluence of lifestyle modifications, accurate self‑care techniques, and timely professional intervention constitutes the most efficacious approach to restoring respiratory and ocular homeostasis.
Let us, therefore, commit to these evidence‑based practices, lest we succumb to the chronic malaise of unchecked rhinitis.
Your exposition, while verbose, misrepresents the role of bacterial infection; the majority of sinusitis cases are viral, not bacterial, and indiscriminate antibiotic use fuels resistance. A more precise epidemiological citation would bolster your argument.
People shoudnt ignore the moral duty to keep the air clean.
Indeed, caring for the environment reflects our collective responsibility, and it directly reduces the allergen load that triggers nasal and ocular discomfort.
Oh, so now every sneeze is a lecture on ethics? Let's just wear masks forever and call it a day.
Honestly, the whole thing sounds like a high school biology review-nothing groundbreaking.
For those seeking further guidance, consider consulting a certified allergist who can perform specific IgE testing and tailor a management plan that aligns with your lifestyle and health goals.
Remember, small changes like keeping windows closed on pollen days can make a big difference in how you feel.
If you’re curious about which over‑the‑counter eye drops are safe with nasal sprays, ask your pharmacist-they’ll help you pick options that won’t aggravate your symptoms.