Hormone Therapy Medication Interaction Checker
Check Your Medications
Separate each medication with a comma (e.g., "aspirin, lisinopril, fluoxetine")
Why This Matters
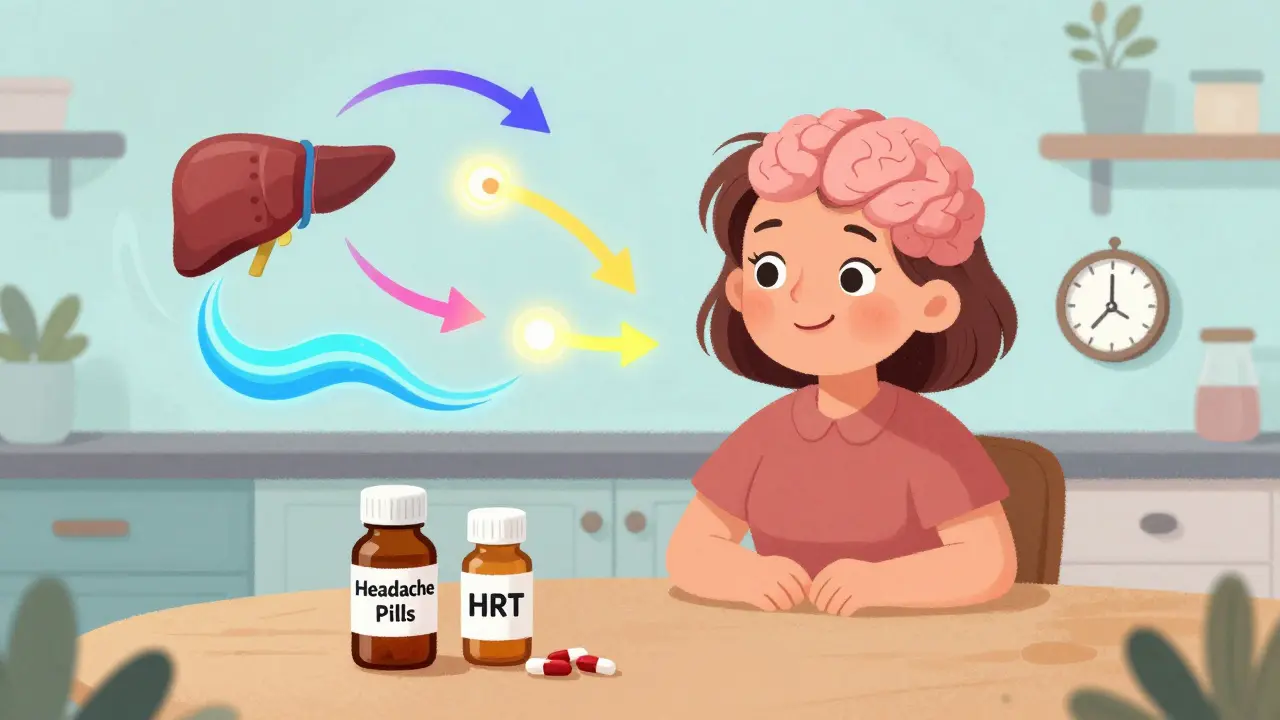
Hormones affect liver enzymes that process your medications. Oral hormone therapy can slow down how your body clears drugs like antidepressants, blood thinners, and statins, potentially causing side effects. Transdermal delivery (patches/gels) avoids this risk by bypassing the liver.
Article insight: "Transdermal patches and gels are becoming more popular because they avoid the liver entirely. This reduces the risk of blood clots and liver strain." (BJOG study, 2022)
Key Interactions
Oral estrogen can increase blood thinning effects, raising bleeding risk
Oral estrogen may slow SSRI metabolism, increasing side effects
Oral estrogen may increase statin blood levels, raising muscle pain risk
Results
Enter your medications and select your delivery method to see potential interactions.
When menopause hits, your body doesn’t just stop having periods-it starts rewiring how it responds to everything, including the medicines you take. What used to be a harmless pill for headaches or high blood pressure might now cause dizziness, nausea, or even mood swings you didn’t expect. The reason? Hormone levels are shifting dramatically, and that changes how your body processes drugs. This isn’t just about hot flashes anymore. It’s about how your liver, kidneys, and brain are now working differently under new hormonal conditions.
How Hormone Therapy Changes How Your Body Handles Medications
Estrogen and progesterone don’t just affect your temperature or mood-they interact with enzymes in your liver that break down medications. When you start hormone replacement therapy (HRT), those enzymes get activated or suppressed. For example, oral estrogen can slow down how quickly your body clears certain antidepressants, blood thinners, and even statins. That means a dose that was safe last year might now build up in your system and cause side effects.
Transdermal patches and gels are becoming more popular because they avoid the liver entirely. Instead of going through digestion, the hormones get absorbed through the skin. This reduces the risk of blood clots and liver strain. A 2022 BJOG study found switching from pills to patches cut gastrointestinal side effects by 60%. If you’re on other meds and suddenly feel off, it might not be the HRT itself-it could be how the HRT is changing your body’s handling of everything else.
Common Side Effects of Hormone Therapy-And When to Worry
Most women on HRT experience mild side effects at first. About 30-50% notice vaginal spotting or bleeding in the first three to six months. That’s normal as your lining adjusts. Breast tenderness? Happens in 20-40% of users. Bloating and headaches? Common, affecting 15-25% and 10-20% respectively. These usually fade after a few months.
But some symptoms aren’t just annoying-they’re warning signs. If you have sudden chest pain, shortness of breath, or swelling in one leg, get checked immediately. These could mean a blood clot. Stroke symptoms like slurred speech or facial drooping need emergency care. The Women’s Health Initiative study showed HRT increases stroke risk by 41% and blood clots by 113% in some women, especially those over 60 or starting therapy more than 10 years after menopause.
And then there’s the breast cancer risk. For women using combination HRT (estrogen + progestin), the absolute risk goes from about 30 cases per 10,000 women to 38 per 10,000 after five years. That’s a small increase, but it matters if you have a family history or BRCA mutations. The key is knowing your personal risk before starting.
Who Should Avoid Hormone Therapy Altogether
Not everyone is a candidate. If you’ve had breast cancer, endometrial cancer, a history of stroke, heart attack, or blood clots, hormone therapy is generally off-limits. The American College of Obstetricians and Gynecologists (ACOG) is clear: these conditions make the risks too high. Liver disease is another red flag-your liver can’t handle the extra load.
Even if you’re otherwise healthy, timing matters. Starting HRT after age 60 or more than 10 years after your last period increases cardiovascular risks by 24%. That’s why experts now talk about the “window of opportunity”-starting early, when your body still responds well to estrogen, gives you the best benefit-to-risk balance.

Alternatives to Hormone Therapy That Actually Work
If HRT isn’t right for you, you’re not out of options. Nonhormonal treatments are more effective than many people realize. SSRIs like paroxetine (Paxil) reduce hot flashes by 50-60% in 60% of users. Gabapentin, often used for nerve pain, cuts hot flashes by 45%. Clonidine, a blood pressure drug, works for about 46% of women. These aren’t magic bullets, but they’re real tools.
For vaginal dryness and painful sex, over-the-counter moisturizers and lubricants help 45% of women. But if those don’t cut it, a low-dose vaginal DHEA insert (Intrarosa) improves sexual pain in 70% of users with almost no systemic absorption. That means no increased risk of clots or cancer-just local relief.
And then there’s fezolinetant, a new drug currently under FDA review. In a 2022 trial, it cut moderate-to-severe hot flashes by over 50%, compared to just 28% with placebo. If approved, it could be a game-changer for women who can’t take hormones at all.
How to Adjust Your Treatment If Side Effects Hit
Side effects don’t mean you have to quit. Most can be fixed with small tweaks. A 2021 Menopause journal study found 68% of women found relief just by adjusting their dose. Maybe you’re on 1 mg of estrogen and your body needs 0.5 mg. Or maybe you’re on a pill and your stomach can’t handle it-switching to a patch solves 45% of those cases.
Here’s what to try in order:
- Wait 3 months. Many side effects fade with time.
- Lower the dose. Start with the smallest effective amount.
- Change the delivery method. Patches or gels avoid liver metabolism and reduce nausea and bloating.
- Switch from combined to estrogen-only-if you’ve had a hysterectomy.
- Try a different progestin. Some, like micronized progesterone, cause fewer mood swings than synthetic versions.
If you miss a pill, don’t double up. Take it as soon as you remember, but skip it if it’s almost time for the next dose. Taking two pills at once can spike hormone levels and trigger spotting or headaches.
What You Need to Tell Your Doctor Before Starting
Before you even think about HRT, list everything you’re taking. That includes over-the-counter meds, supplements, and herbal products. Some-like St. John’s wort or black cohosh-can interfere with hormone therapy. Black cohosh, for example, showed mixed results in 12 trials involving nearly 2,000 women. No one knows how it interacts with prescription drugs.
Also, share your full medical history: surgeries, blood clots, migraines with aura, high blood pressure, or family history of cancer. Even if you think it’s unrelated, it might change your options. Your doctor might suggest a low-dose vaginal estrogen instead of systemic therapy, or recommend nonhormonal options first.
The Big Picture: Is HRT Worth It for You?
The decision isn’t about whether HRT is safe or dangerous. It’s about whether it’s right for you-right now. For a 52-year-old woman with severe hot flashes, night sweats, and insomnia, HRT might restore her sleep, her mood, and her ability to work. For a 65-year-old with a history of clots, the risks outweigh the benefits.
Use this rule of thumb: If you’re under 60 and within 10 years of menopause, and your symptoms are disrupting your life, the benefits usually outweigh the risks. If you’re older or have risk factors, explore nonhormonal options first.
And remember: you’re not alone. About 75% of women have menopause symptoms. One in four has severe ones. You don’t have to suffer in silence. But you do need to be informed. Talk to your doctor. Ask about alternatives. Track your symptoms. And don’t be afraid to change course if something isn’t working.
Can hormone therapy cause weight gain?
Hormone therapy itself doesn’t directly cause weight gain. But menopause does-lower estrogen changes where your body stores fat, often pushing it toward the abdomen. Some women notice bloating from fluid retention on HRT, which can feel like weight gain. This usually improves after a few months. The real issue is metabolism slowing down with age, not the hormones.
How long should I stay on hormone therapy?
There’s no fixed timeline. Most women use it for 2-5 years to manage symptoms. Some need it longer, especially if symptoms persist past 60. The key is using the lowest dose for the shortest time needed. Annual check-ins with your doctor help decide if you can reduce or stop safely. Stopping suddenly can cause symptoms to return sharply.
Are bioidentical hormones safer than traditional HRT?
No. Bioidentical hormones are marketed as “natural” and safer, but they’re not FDA-regulated like standard HRT. Compounded versions can have inconsistent dosing, increasing risks. The FDA and ACOG warn against them because there’s no proof they’re safer or more effective. Stick to FDA-approved formulations with proven safety data.
Can I take HRT if I have high blood pressure?
It depends. If your blood pressure is well-controlled, low-dose transdermal estrogen (patches or gels) is often safe. Oral estrogen can raise blood pressure in some women, so it’s usually avoided. Always monitor your BP closely when starting HRT. Your doctor may adjust your antihypertensive meds at the same time.
Do HRT side effects go away on their own?
Yes, most do. Spotting, breast tenderness, bloating, and headaches often fade within 3-6 months as your body adjusts. If they last longer or get worse, it’s not normal. Don’t ignore them-talk to your doctor. You might need a dose change or a different delivery method.
What’s the best way to stop hormone therapy?
Don’t quit cold turkey. Gradually lowering the dose over 2-3 months helps avoid a rebound of hot flashes and mood swings. For example, switch from a 1 mg pill to a 0.5 mg, then take it every other day for a month before stopping. Work with your doctor to create a tapering plan. If symptoms return badly, you might need to restart at a lower dose.





14 Comments
Ugh, I swear every doctor acts like HRT is the only solution. I’ve been on gabapentin for 8 months and my hot flashes are GONE. Why do they keep pushing pills when non-hormonal stuff works better? 😒
Actually, the 2022 BJOG study you mentioned? It was a retrospective cohort, not RCT. Also, 60% reduction in GI side effects? That’s not even statistically significant when you account for attrition bias. 🤓 Just saying - don’t trust headlines.
They don’t want you to know this - but HRT is just Phase 3 of the Big Pharma mind control program. Estrogen? It’s a synthetic endocrine disruptor designed to keep women docile. The liver enzyme suppression? That’s not side effect - that’s surveillance. You think your ‘mood swings’ are natural? Nah. It’s the pills. They’re watching your serotonin levels through your prescriptions. 🕵️♂️💊
You got this!! 💪 HRT isn’t for everyone, but if it helps you sleep and stop crying at commercials - go for it. Your quality of life > random stats. 🌸
I was so scared to start HRT after reading all the scary stuff online. But my doctor helped me start low and slow - patch, 0.5mg. After 2 months, I felt like myself again. I cried happy tears. You’re not alone. 🤍
This is one of the most balanced, well-researched pieces on menopause I’ve read in years. The distinction between transdermal and oral is crucial - most people don’t get that. Thank you for writing this. 🙏
Just switched from pill to gel last week and the bloating disappeared in 3 days. Also stopped taking that gummy vitamin with black cohosh - no idea how it was interacting but my headaches got worse. Lesson learned: always tell your doc EVERYTHING. Even the weird teas.
Bioidentical hormones? Please. The word ‘natural’ is the most dangerous word in medicine. Just because it comes from a plant doesn’t mean it’s safe - or even regulated. The FDA warnings exist for a reason. Don’t be fooled by Instagram influencers selling ‘hormone magic’.
Wow, so you’re just gonna hand out hormone prescriptions like candy? What about the women who’ve had breast cancer? You’re basically saying ‘just take it if you’re young enough’ - but what if you’re 58 and your mom died of estrogen-positive cancer at 59? You think your ‘window of opportunity’ is more important than genetic risk? 🤦♂️
So… you’re telling me the same pill that gives me a headache also keeps me from crying in Target? Sign me up. 😅
I’ve been on HRT for 7 years and I’ve gained 30 lbs, my anxiety is through the roof, and my husband says I’ve become a different person. But hey - at least I don’t have hot flashes anymore. So… is it worth it? I don’t know anymore. I just feel like a lab rat. Everyone says ‘it’s normal’ but no one tells you what it costs. 🥲
Dear author, I am from India and I have been suffering from menopausal symptoms for 3 years. I have tried Ayurveda, homeopathy, yoga, and meditation. I do not believe in Western medicine. Please advise me on non-pharmaceutical alternatives that are scientifically validated. Thank you.
As a woman of color who grew up with grandmothers who used herbal teas and cold compresses, I appreciate that this article acknowledges non-hormonal options. But I wish it had included more about cultural approaches - like how some African and Asian communities use yams, moringa, or acupuncture. It’s not just about pills vs patches. It’s about honoring our ancestral knowledge too. 🌿
Just read Deep Rank’s comment - I feel you. I went through that too. The weight gain, the fog, the guilt - it’s real. But I switched to a low-dose patch and added daily walks. Took 4 months but I’m back to 90%. You’re not broken. Just needs tweaking. 💕