Every year, over a million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t caused by bad prescriptions or pharmacy errors-they’re the result of lifestyle habits that make drugs less effective-or more dangerous. The good news? You don’t always need more pills to stay safe. Sometimes, all you need is to change how you eat, move, and rest.
Why Lifestyle Changes Matter More Than You Think
Taking multiple medications is common, especially as we get older. But taking five or more drugs at once-something doctors call polypharmacy-triples your risk of dangerous side effects, falls, confusion, and hospital stays. The problem isn’t just the pills themselves. It’s how your body reacts to them when you’re not giving it the support it needs. Lifestyle changes don’t replace medicine. They make medicine work better. Research from JAMA Internal Medicine, which looked at over 3.4 million people, found that people who made consistent lifestyle changes reduced their need for medication by 25% to 50% for conditions like high blood pressure, diabetes, and high cholesterol. That’s not a small win. It means fewer pills, fewer interactions, and fewer trips to the hospital.Move More-Even Just a Little
You don’t need to run marathons. You don’t even need to join a gym. Just walking briskly for 30 minutes, three days a week, can make a real difference. This kind of movement strengthens your heart, lowers blood pressure, and helps your body use insulin better. One study showed that people with high blood pressure who walked regularly lowered their numbers as much as those taking a single blood pressure pill. That’s not a coincidence. When your heart gets stronger, it doesn’t have to work as hard. That means your body may not need as much medication to keep pressure under control. The American Heart Association recommends 150 minutes of moderate exercise per week. That’s 30 minutes, five days a week. If that feels too much, start with 10 minutes a day. Build up slowly. Add a few extra steps each week. Even small increases in activity can reduce your need for statins, beta-blockers, or diuretics over time.Eat to Support Your Meds, Not Fight Them
What you eat can either help your medication work-or block it completely. For high blood pressure, cutting back on sodium is one of the most powerful moves you can make. The DASH diet (Dietary Approaches to Stop Hypertension), which focuses on vegetables, fruits, whole grains, and lean proteins, can lower blood pressure as much as a single prescription drug. One study found that switching to DASH and reducing salt lowered systolic pressure by 11 points and diastolic by 5 points-right in line with what most pills achieve. For Type 2 diabetes, losing just 5% to 7% of your body weight through diet and movement can cut your need for insulin or metformin by up to 60% if you’re prediabetic, and by 40% if you already have the condition. That’s not magic. It’s biology. Less fat around your organs means your body responds better to insulin. But here’s the catch: some healthy foods interfere with meds. Grapefruit, for example, affects 85% of statins, making them too strong and increasing the risk of muscle damage. Leafy greens like spinach and kale are full of vitamin K, which can make blood thinners like warfarin less effective. Dairy products can block the absorption of certain antibiotics. That’s why you need to talk to your pharmacist-not just your doctor. Ask: “Are there any foods I should avoid with my medications?” Don’t assume everything healthy is safe. Some of the most dangerous interactions come from foods people think are good for them.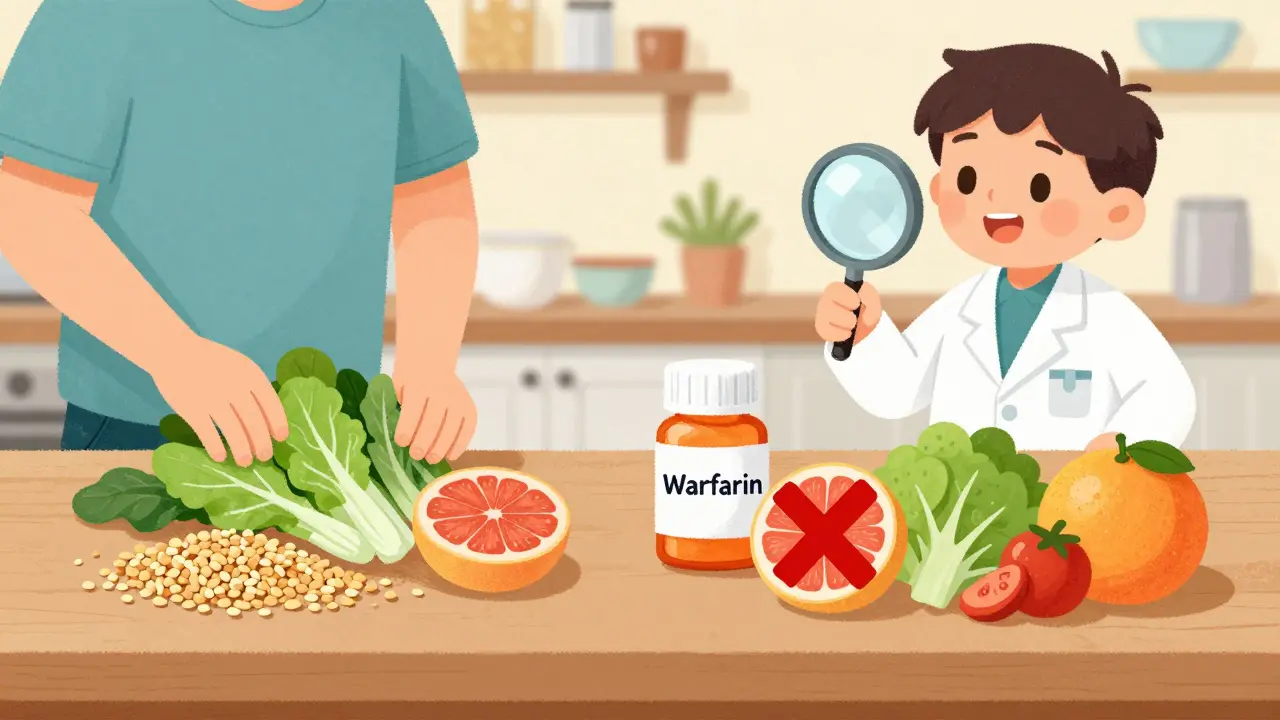
Sleep Isn’t Optional
If you’re sleeping less than seven hours a night, you’re making your medications work harder-and your body more vulnerable. Chronic sleep deprivation is linked to higher blood pressure, insulin resistance, weight gain, and inflammation-all things that make chronic diseases worse. Poor sleep also messes with your body’s ability to process drugs. A 2023 study found that people who slept less than six hours had higher levels of certain medications in their bloodstream, increasing the chance of side effects. Try to get seven to nine hours of quality sleep every night. That means no screens an hour before bed, a cool dark room, and a regular schedule-even on weekends. If you’re snoring or waking up tired, talk to your doctor. Sleep apnea is common, untreated, and makes nearly every medication less effective.Quit Smoking, Cut Back on Alcohol
Smoking doesn’t just hurt your lungs. It makes your heart work harder, raises your blood pressure, and speeds up how fast your body breaks down certain drugs. That means you might need higher doses of medications for conditions like depression, asthma, or even pain-and you’re still at higher risk for heart attacks and strokes. Alcohol is another hidden risk. Drinking more than one drink a day for women or two for men can raise blood pressure, interfere with diabetes meds, and increase liver damage from statins or painkillers. Even moderate drinking can make you dizzy or confused when combined with sedatives or blood pressure pills. Cutting back doesn’t mean going cold turkey. Start by setting limits. Skip alcohol two days a week. Swap one drink for sparkling water with lemon. Small steps add up.Stress Is a Silent Med Killer
Chronic stress raises cortisol, which spikes blood sugar, increases blood pressure, and triggers inflammation. All of this makes your medications less effective. You don’t need to meditate for an hour a day. Start with five minutes. Try deep breathing: inhale for four counts, hold for four, exhale for six. Repeat five times. Do it when you wake up, before bed, or right after taking your pills. Yoga, walking in nature, listening to music, or even journaling for 10 minutes can lower stress enough to help your body respond better to treatment. One study found that people who practiced mindfulness for eight weeks lowered their blood pressure as much as those on a first-line antihypertensive drug.
Give It Time-And Track Progress
Lifestyle changes don’t work overnight. Unlike a pill that lowers your blood pressure in hours, a better diet or walking routine takes weeks to show results. Most people start seeing changes in 3 to 6 months. Keep a simple log: write down what you ate, how much you walked, and how many hours you slept each day. Use a free app if it helps. Don’t aim for perfection. Aim for consistency. One person on Reddit shared that after six months of walking daily and cutting salt from 3,500mg to 1,500mg, their blood pressure dropped from 150/95 to 125/80. Their doctor took them off one pill. That’s the kind of win that happens when you stick with it.Never Stop Taking Meds Without Talking to Your Doctor
This is critical: lifestyle changes should never be used to stop or reduce your medication on your own. Abruptly stopping blood pressure pills, diabetes meds, or antidepressants can be deadly. Work with your doctor. Tell them what you’re doing. Ask: “Can we monitor my numbers over the next few months and see if we can safely lower my dose?” Many doctors are now trained in lifestyle medicine and welcome this kind of collaboration. The American College of Lifestyle Medicine has over 12,000 certified practitioners worldwide. Some clinics even offer structured programs that combine nutrition coaching, exercise plans, and medication reviews-all in one place.Real Progress, Real Results
People who combine smart lifestyle habits with their medications don’t just take fewer pills. They feel better. They have more energy. They sleep better. They worry less. A survey by the American Heart Association found that 68% of people with chronic conditions said their quality of life improved after making lifestyle changes. Only 32% struggled to keep going. That’s a big gap. And the ones who stuck with it? They didn’t rely on willpower. They built habits. Start with one thing. Walk three days this week. Cut salt in half. Go to bed 30 minutes earlier. Talk to your pharmacist about food-drug interactions. Medications save lives. But your daily choices? They’re the foundation that makes those lives worth living.Can lifestyle changes really replace my medication?
No. Lifestyle changes should never replace medication without your doctor’s guidance. They work best alongside your prescriptions, helping them work more effectively and sometimes allowing for lower doses over time. Stopping meds on your own can be dangerous.
How long does it take to see results from lifestyle changes?
Most people start seeing measurable improvements in blood pressure, blood sugar, or cholesterol after 3 to 6 months of consistent effort. Some changes, like better sleep or reduced stress, may show up sooner-within a few weeks. But lasting results require patience and steady habits.
What foods should I avoid while taking medication?
Grapefruit interferes with 85% of statins and some blood pressure meds. Leafy greens like spinach and kale can reduce the effect of warfarin. Dairy can block absorption of certain antibiotics. Always ask your pharmacist: "Are there any foods I need to avoid with my specific meds?"
Do I need to exercise every day?
No. The American Heart Association recommends 150 minutes of moderate exercise per week-that’s 30 minutes, five days a week. But even 10 minutes a day helps. Start small. Build up. Consistency matters more than intensity.
Can I still drink alcohol if I’m on medication?
It depends on your meds. Alcohol can raise blood pressure, interfere with diabetes drugs, and increase liver damage from statins or painkillers. For safety, limit to one drink a day for women, two for men-and never mix alcohol with sedatives or anti-anxiety meds.
Why isn’t my doctor talking to me about lifestyle changes?
Many doctors want to discuss lifestyle changes but feel pressed for time or lack training. Don’t wait for them to bring it up. Ask: "What lifestyle changes would help me reduce my meds safely?" More doctors are now trained in lifestyle medicine-ask if your clinic offers it.
What if I can’t stick to a diet or exercise plan?
Start with one tiny habit. Walk after dinner. Swap soda for sparkling water. Go to bed 15 minutes earlier. Don’t try to overhaul everything at once. Success comes from small, repeatable actions-not perfection. If you miss a day, just start again the next day.
Are there programs that help with lifestyle changes?
Yes. Many employers, Medicare Advantage plans, and community health centers now offer lifestyle medicine programs with nutritionists, exercise coaches, and medication reviews. Look for programs certified by the American College of Lifestyle Medicine-they’re backed by research and designed to work with your meds.






12 Comments
So let me get this straight - I can ditch half my pills if I just walk to the fridge more often? Sign me up. Also, grapefruit is a traitor. I knew I shouldn’t have trusted that shiny little fruit.
Yo, I’ve been doing the DASH diet for 4 months and my bp dropped from 148/92 to 122/80 - no med changes yet, but my doc was shocked. Also, I started using MyFitnessPal to track sodium and now I’m obsessed. It’s like a game. #lifestylehacking
Actually, the JAMA study you cited had a confounding variable: adherence bias. People who self-report lifestyle changes are already more health-literate and likely have better access to care. The causal inference is shaky without RCTs controlling for SES. Also, vitamin K antagonism with warfarin is well-documented since the 1950s - not exactly groundbreaking.
For anyone feeling overwhelmed - start with one thing. I used to hate walking, so I started by just stepping outside after my morning coffee. Five minutes. Then ten. Now I do 20. No gym. No fancy gear. Just me, my shoes, and the birds. You don’t need to be perfect. You just need to show up. And you’re already here - that counts.
I just want to say - this is so important - I’ve seen so many people in my community - elderly folks, single moms, veterans - who are just drowning in pills because no one ever taught them that food is medicine - and sleep isn’t a luxury - it’s a biological necessity - and stress isn’t ‘all in your head’ - it’s literally rewiring your hormones - and I’m so glad someone finally wrote this - because the system is broken - and we’re all just trying to survive - and this - this right here - is hope - not a pill - but a habit - a daily choice - a walk - a breath - a quiet night - please - if you take one thing from this - let it be that you are not broken - you just need support - not more meds - just more care.
Pathetic. You’re glorifying basic biochemistry as if it’s revolutionary. Of course diet affects drug metabolism. This is Med 101. Why is this even a viral post?
There’s something quietly beautiful about the idea that healing doesn’t always come in a bottle. Sometimes it’s the smell of rain on pavement after a walk. The way your shoulders drop when you finally stop scrolling before bed. The silence between breaths. These aren’t ‘lifestyle hacks’ - they’re acts of rebellion against a system that sells you pills instead of peace. I’m not saying ditch your meds. I’m saying: don’t let the medicine become your only relationship with your body.
lol i tried the 10-min walk thing… then i remembered i forgot to take my blood pressure pill that morning so i just sat on the couch and cried. then i ate a bag of chips. but hey - at least i didn’t drink. maybe tomorrow.
Bro this is the most real post I’ve read in months. I’m from India and we don’t talk about this stuff. My dad is on 7 meds and we just give him pills like candy. I’m going to start cooking him dal and greens and make him walk after dinner. No more TV after 8. He’s 68. He deserves better.
Thank you for this thoughtful, well-researched, and compassionate guide. Your emphasis on collaboration with healthcare providers is not only prudent - it is essential. I have shared this with my senior center group, and we are forming a weekly walking circle. Small steps, indeed. With gratitude and respect.
Typical liberal nonsense. You want people to walk instead of take meds? What about the veterans who need their pills to survive? This is dangerous. Stop pushing your agenda. Pills save lives. Not yoga.
Interesting. But you didn’t mention the placebo effect of ‘lifestyle change’ narratives. People who believe they’re ‘doing better’ often report improved biomarkers - regardless of actual physiological change. Also, the DASH diet is just low-sodium. We’ve known that since the 80s. This reads like a wellness influencer’s LinkedIn post.