Candida auris – Quick Facts, Symptoms, and How to Stay Safe
Candida auris is a yeast that can cause tough infections, especially in hospitals. Unlike common yeast infections, it can survive on surfaces for weeks and resist many drugs. That’s why it’s making headlines worldwide.
Most people who get sick with candida auris have an underlying health issue – recent surgery, a weakened immune system, or a long stay in a care facility. If you’re healthy and stay home, the risk is very low.
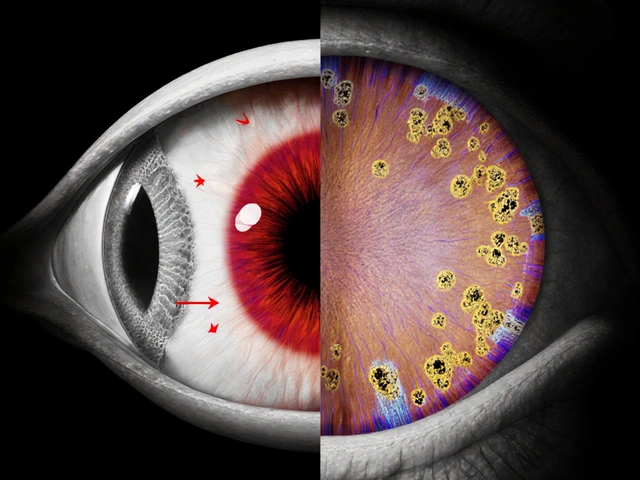
How It Spreads and What It Looks Like
Think of candida auris like a stubborn stain. It spreads through direct contact with contaminated skin, medical equipment, or even a dirty hospital room. It doesn’t jump from person to person the way a cold does, but touching a surface that’s been contaminated can pass it on.
Symptoms often mimic other infections, which makes it tricky to spot. Look for fever, chills, and a feeling of being very sick. In some cases, the infection appears as a wound that won’t heal, a urinary tract infection, or a bloodstream infection that can cause organ failure. If you notice any of these signs after a hospital stay, tell your doctor right away.
Diagnosing and Treating Candida auris
Because candida auris looks like other yeasts under a microscope, labs need special tests to confirm it. Your doctor may send a sample to a reference laboratory that can run the right test.
Treatment is tricky: many standard antifungal drugs don’t work. Doctors usually start with an echinocandin, a newer class of antifungal that works better against candida auris. If the infection is caught early, the chances of recovery improve dramatically.
Even after treatment, doctors will keep a close eye on you with follow‑up cultures. The fungus can hide and come back if not fully cleared.
Practical Steps to Keep You and Your Loved Ones Safe
Most of the time, the best protection happens in health‑care settings. Here’s what you can do:
- Ask staff to wash their hands before touching you. Hand hygiene is the single most effective tool.
- Make sure any equipment (like catheters or breathing tubes) is cleaned or replaced according to hospital protocol.
- If you’re being discharged, request a clean environment for your home recovery. Candida auris can survive on doorknobs, bedside tables, and even towels.
- Wash your hands with soap and water for at least 20 seconds before and after caring for a wound or using the bathroom.
- Don’t share personal items – towels, razors, or socks – with someone who might be infected.
At home, regular cleaning with an EPA‑approved disinfectant works well. Focus on high‑touch surfaces like light switches, phones, and bathroom fixtures.
If you’re a caregiver, wear gloves when you’re cleaning or changing dressings, and dispose of them safely.
What’s New in the Fight Against Candida auris?
Researchers are racing to develop faster tests and new drugs that can beat resistant strains. Some hospitals are already using rapid DNA testing that spots the fungus within hours, cutting the time it takes to start the right treatment.
Public health agencies are tracking outbreaks and sharing guidelines with facilities across the country. Staying informed about local alerts can help you ask the right questions if you’re admitted to a hospital.
In short, candida auris is a serious but manageable problem when you know the signs and take simple steps to prevent it. Keep an eye on any infection after a medical stay, practice good hand hygiene, and don’t hesitate to ask health‑care providers about their cleaning protocols. Staying aware is the best defense.