Respiratory Depression Risk Calculator
How Your Combination Affects Your Risk
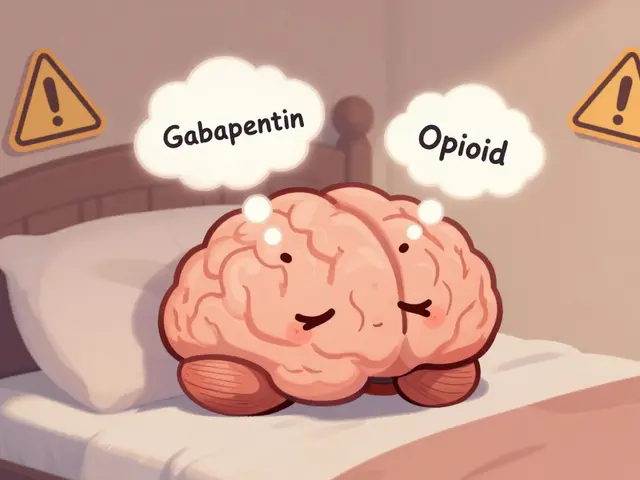
This tool calculates your risk of respiratory depression when taking gabapentinoids (gabapentin or pregabalin) with opioids. Based on FDA and MHRA guidelines, this combination can cause dangerous breathing problems, especially at higher doses or with certain risk factors.
When you take gabapentin or pregabalin for nerve pain, and your doctor adds an opioid like oxycodone or morphine for extra relief, you might think you’re getting better control over your symptoms. But what you don’t see is the quiet, creeping danger: respiratory depression. This isn’t just a theoretical risk-it’s a documented, deadly interaction that’s killed people in hospitals and at home, often without warning.
What Happens When Gabapentinoids Meet Opioids?
Gabapentinoids-gabapentin (Neurontin, Gralise) and pregabalin (Lyrica)-were never meant to be paired with opioids. They were designed to calm overactive nerves, not to slow breathing. But when they’re taken together, something dangerous happens: both drugs hit the same control center in your brainstem-the part that tells your lungs when to breathe. It’s like turning down two volume knobs at once. One might be quiet. Two? Silence. The U.S. Food and Drug Administration (FDA) looked at over 100,000 adverse event reports between 2012 and 2017 and found 49 cases of serious breathing problems linked to gabapentinoids. Ninety-two percent of those cases involved either another CNS depressant (like an opioid) or an existing breathing problem like COPD or sleep apnea. Twelve of those cases ended in death. All 12 had at least one risk factor. It’s not just about opioids. Alcohol, benzodiazepines, and even some sleep aids can make this worse. But opioids are the most common partner in this deadly mix. In one large study of over 16 years of patient data, people taking both gabapentin and an opioid had a 50% higher chance of dying from an opioid-related cause. For those on very high doses of gabapentin, that risk nearly doubled.Why Does This Happen?
It’s not just additive. It’s more complex than simply adding two sedatives together. Gabapentinoids can actually reverse some of the tolerance your body builds to opioids. That means if you’ve been on opioids for a while and your body has adjusted, adding gabapentin can suddenly make you as sensitive to opioids as someone who’s never taken them before. Your body thinks it’s safe to breathe slower-but it’s not. There’s also a physical reason. Opioids slow down your gut. That means gabapentin, which is absorbed mostly in the upper small intestine, sits there longer. More of it gets absorbed. Higher blood levels. More sedation. More risk. Studies with healthy volunteers confirm this. One trial gave people pregabalin and remifentanil (a fast-acting opioid) separately and together. When combined, their carbon dioxide levels rose-meaning their breathing was less effective. Another study found that even a single dose of gabapentin increased the number of apnea episodes (pauses in breathing) during sleep by more than double compared to placebo.Who’s at the Highest Risk?
This isn’t a risk that affects everyone equally. Certain people are far more vulnerable:- People over 65-aging lungs and brains are less resilient.
- Those with kidney problems-gabapentin and pregabalin are cleared by the kidneys. If your kidneys aren’t working well, the drugs build up.
- Patients with COPD, asthma, or sleep apnea-their breathing is already compromised.
- People on high doses-doses over 1,800 mg of gabapentin or 300 mg of pregabalin daily carry significantly higher risk.
- Post-surgery patients-especially after major procedures like heart or chest surgery, where respiratory depression rates jump to 17% or higher when gabapentinoids are added.

The Myth of the Opioid-Sparing Drug
Many doctors started prescribing gabapentinoids in the 2010s as a way to reduce opioid use. It made sense: less opioid = less addiction risk. But the data doesn’t support this strategy when it comes to pain control. A 2020 analysis of over 5.5 million surgical patients found no strong evidence that adding gabapentinoids improves pain relief when used with opioids. In fact, the benefits were described as “equivocal.” That means you’re not getting better pain control-you’re just adding a new, potentially fatal risk. The rise in co-prescribing is alarming. In 2017, nearly one in five new gabapentin prescriptions came with an opioid. That’s not accidental. It’s a pattern born from good intentions-trying to reduce opioid dependence-but it’s backfiring.What Should You Do?
If you’re taking both gabapentin and an opioid, talk to your doctor. Don’t stop suddenly-withdrawal from either can be dangerous. But do ask:- Is this combination truly necessary?
- Could I try a non-sedating alternative for nerve pain, like duloxetine or amitriptyline?
- Am I on the lowest effective dose of both drugs?
- Have my kidney function and breathing been checked recently?

How to Reduce the Risk
If your doctor decides the combination is still needed, follow these steps:- Start low, go slow. Begin with the smallest possible dose of gabapentinoid-often 100 mg of gabapentin or 25 mg of pregabalin once a day.
- Check kidney function. If your creatinine clearance is below 60 mL/min, your dose must be reduced. Pregabalin needs adjustment at 60; gabapentin at 70.
- Avoid high doses. Doses above 1,800 mg gabapentin or 300 mg pregabalin daily should only be used in rare cases, with close monitoring.
- Never combine with alcohol or benzodiazepines. These make the risk exponentially worse.
- Use the lowest effective opioid dose. If you’re on more than 50 mg morphine equivalent per day, the risk rises sharply.
The Bigger Picture
This isn’t just about two drugs. It’s about how our healthcare system handles pain. We’ve been so focused on avoiding opioids that we’ve turned to alternatives without fully understanding their dangers. Gabapentinoids are not harmless. They’re potent CNS depressants with a hidden profile. Regulators have sounded the alarm. The FDA and MHRA have updated labels. But prescriptions haven’t dropped. In fact, gabapentinoid use has continued to climb, especially in older adults and those with chronic pain. The truth is, we need better tools. We need decision support systems in electronic health records that flag dangerous combinations. We need clearer guidelines for primary care doctors who aren’t pain specialists. And we need patients to speak up-if you’re feeling unusually sleepy or short of breath, say something.What Are the Alternatives?
For neuropathic pain, there are other options that don’t carry the same respiratory risk:- Duloxetine (Cymbalta)-an SNRI antidepressant with strong evidence for diabetic nerve pain.
- Amitriptyline-a low-dose tricyclic antidepressant, often effective and cheaper.
- Topical lidocaine or capsaicin-for localized pain, no systemic effects.
- Cognitive behavioral therapy (CBT)-proven to reduce pain perception over time.
- Physical therapy and movement-often more effective than pills for chronic nerve pain.
Can gabapentin alone cause respiratory depression?
Yes. While the risk is much higher when combined with opioids or other sedatives, studies and regulatory agencies like the FDA and MHRA have confirmed that gabapentin and pregabalin alone can cause respiratory depression, especially in older adults, those with kidney disease, or people with pre-existing lung conditions. Even in healthy individuals, single doses have been shown to increase breathing pauses during sleep.
How do I know if I’m at risk for respiratory depression?
You’re at higher risk if you’re over 65, have kidney disease, COPD, asthma, sleep apnea, or are taking other sedatives like benzodiazepines, alcohol, or opioids. If you’ve been on gabapentinoids for more than a few weeks and feel unusually tired, confused, or short of breath-even mildly-you should get checked. A simple oxygen saturation test can reveal if your breathing is being affected.
Is it safe to take gabapentin with a low-dose opioid like codeine?
No. There’s no safe threshold. Even low-dose opioids combined with gabapentin increase the risk of respiratory depression. The interaction isn’t linear-it’s unpredictable. One person might tolerate it, another might stop breathing. The FDA and MHRA warn against this combination regardless of dose. Safer alternatives exist for pain relief.
Why are gabapentinoids still prescribed with opioids if the risk is so high?
Because many doctors believe they reduce opioid needs, even though studies show they don’t improve pain control. The rise in co-prescribing started during the opioid crisis, when clinicians were pressured to cut opioid doses. Gabapentinoids seemed like a safe substitute-but they’re not. Poor awareness, lack of training, and outdated prescribing habits keep this dangerous practice alive.
What should I do if I’m already taking both drugs?
Don’t stop suddenly. Contact your doctor to review your medications. Ask if you really need both, whether your dose is the lowest possible, and if your kidney function has been checked. Consider switching to non-sedating alternatives like duloxetine or topical treatments. If you’re experiencing drowsiness, confusion, or shallow breathing, seek medical help immediately.
Respiratory depression doesn’t announce itself with a scream. It creeps in quietly-slower breaths, deeper sleep, a foggy mind. By the time it’s obvious, it’s often too late. The combination of gabapentinoids and opioids is one of the most underrecognized killers in modern pain management. You don’t need to live with that risk. There are safer ways to manage pain. Ask for them.



14 Comments
i just started taking gabapentin for my sciatica and my dr threw in a little oxycodone for "extra help"... i had no idea this could be deadly. i feel like i just got handed a time bomb with a prescription label. 😳
This is an incredibly important public health alert. The combination of gabapentinoids and opioids represents a silent epidemic that has been overlooked due to well-intentioned but misguided pain management practices. Healthcare providers must be better educated, and patients must be empowered with clear, accessible information.
I’m so glad someone finally said this out loud... my mom was on both for years after her back surgery, and we never knew why she kept nodding off at dinner... now it all makes sense. Please, if you’re reading this and you’re on this combo, talk to your doctor. Don’t wait until it’s too late. 💔
Ah, the neoliberal pharmacopeia in full bloom. A bio-political cascade of pharmaceutical commodification, where the body is reduced to a pharmacokinetic variable, and the physician becomes a mere conduit for corporate formularies. The opioid crisis was never about addiction-it was about the collapse of phenomenological care into algorithmic prescribing. Gabapentinoids? Merely the latest ontological extension of the medical-industrial complex’s necropolitical logic.
People think these drugs are safe because they are not heroin. But the truth is, every time you take something that slows your breathing, you are playing russian roulette. I have seen too many people die from this. No excuses. No exceptions. Stop mixing them. End of story.
This is why America is falling apart. Doctors give out pills like candy and then act surprised when people die. We don’t need more studies-we need less prescribing. Stop letting foreigners and lazy MDs ruin our health with this nonsense.
The brainstem doesn't care about your pain. It cares about CO2 levels. When you layer CNS depressants, you're not managing pain-you're overriding homeostasis. This isn't a side effect. It's a system failure. And we're all complicit because we want the easy fix.
my grandma took this combo and passed in her sleep... no one knew why. i still cry about it. please check on your loved ones. 🕊️
I’ve been on gabapentin for 5 years and just started opioids last year for a flare-up. I’ve been feeling weirdly tired lately but thought it was just stress. Now I’m scheduling a blood test and a chat with my doc. Better safe than sorry, right?
The clinical evidence is unequivocal. Co-prescribing gabapentinoids with opioids increases mortality risk in a dose-dependent manner. Clinical guidelines must be enforced, and electronic health record alerts should be mandatory.
There’s a deeper philosophical question here: if we treat pain as a problem to be eliminated rather than a signal to be understood, we’ve already lost. We’ve outsourced our suffering to chemistry, and now we’re surprised when the chemistry turns against us. The body doesn’t lie-it just gets louder when we stop listening. Maybe the real question isn’t how to avoid respiratory depression, but why we’re so desperate to silence pain in the first place.
I was skeptical at first but after reading this i went back and checked my meds-turns out i was on 2400mg gabapentin + 30mg oxycodone. holy crap. i called my dr today and we’re cutting both down. you guys are lifesavers. 🙏
I wonder how many of these deaths are being misclassified as cardiac arrest or overdose without the gabapentinoid factor being noted. It’s a silent killer because the system doesn’t look for it.
The FDA’s data is alarming, but it’s only the tip of the iceberg. Most adverse events go unreported, especially in elderly patients who can’t advocate for themselves. Add in the fact that gabapentinoids are often prescribed by PCPs with no pain management training, and you’ve got a perfect storm. We need mandatory CME modules on CNS depressant interactions-and not just for prescribers, but for pharmacists too. This isn’t just about individual choices; it’s about systemic failure. We’ve normalized dangerous polypharmacy under the guise of patient-centered care, and it’s costing lives. The alternatives exist. The evidence is clear. The question is: who’s going to act before another 12 people die?