Opioid Rotation Calculator
Calculate Equivalent Dose
Find the proper starting dose when switching opioids. This tool applies medical guidelines for safe rotation.
Results
Important: This calculation applies the standard 25-50% safety margin per clinical guidelines.
Methadone requires special caution - monitor closely for 10 days.
Always consult your physician before switching opioids.
When pain medication stops working-or starts making things worse-many patients face a hard choice: take more pills and risk worse side effects, or find another way. For people on long-term opioids, opioid rotation isn’t just an option-it’s often the smartest next step. This isn’t about giving up on pain control. It’s about switching to a different opioid to keep the pain managed while cutting down on nausea, drowsiness, confusion, or constipation that no one should have to live with.
Why Switch Opioids at All?
Not all opioids work the same way in every body. Just because morphine gives you terrible nausea doesn’t mean oxycodone or fentanyl will too. The body doesn’t respond to all opioids equally. One person might tolerate codeine fine but get dizzy on hydrocodone. Another might need high doses of oxycodone to feel relief, but switch to methadone and suddenly need half the dose with better control. This isn’t luck-it’s pharmacology. The goal of opioid rotation isn’t to increase the dose. It’s to find a better fit. Studies show that between 50% and 90% of patients see improvements in side effects-or even better pain control-after switching. That’s not a small number. It’s the majority.When Is Opioid Rotation Recommended?
Doctors don’t switch opioids just because a patient is tired of their current pill. There are clear, evidence-based reasons:- Intolerable side effects: Nausea, vomiting, drowsiness, confusion, muscle twitching, or hallucinations that don’t go away even after trying anti-nausea meds or adjusting the dose.
- Poor pain control despite high doses: If you’ve doubled or tripled your dose and your pain hasn’t improved, you’re likely hitting a wall-not a solution.
- Drug interactions: If you’re starting a new medication (like an antidepressant or seizure drug) that doesn’t mix well with your current opioid, rotation can avoid dangerous reactions.
- Changing health status: Liver or kidney problems can change how your body processes opioids. A drug that was safe last year might be risky now.
- Need for a different route: If swallowing pills becomes hard (due to nausea, swallowing issues, or surgery), switching to a patch, injection, or suppository may be necessary.
It’s important to know what doesn’t count as a reason. A sudden spike in pain after an injury? That’s a pain crisis, not a reason to rotate. It needs immediate, targeted care-not a drug swap.
The Myth of ‘Opioid Resistance’
Some patients are told they’re “resistant to opioids.” That’s misleading. You’re not resistant to all opioids-you’re resistant to this one. Think of it like antibiotics. If amoxicillin doesn’t clear your infection, you don’t say you’re resistant to all antibiotics. You try a different one. Same with opioids.The 2009 expert guidelines from the Journal of Pain and Symptom Management specifically warned against using the term “poor opioid responsiveness.” It’s inaccurate and can lead to under-treatment. The real issue is mismatched drug and patient-not patient failure.
Which Opioids Work Best for Reducing Side Effects?
Not all switches are equal. Some substitutions have proven better for certain side effects:- Oxycodone: Often better than morphine for nausea and constipation. Many patients report clearer thinking and less drowsiness.
- Fentanyl (patch or lozenge): Useful when oral intake is difficult. Less likely to cause gut slowdown, which helps with constipation.
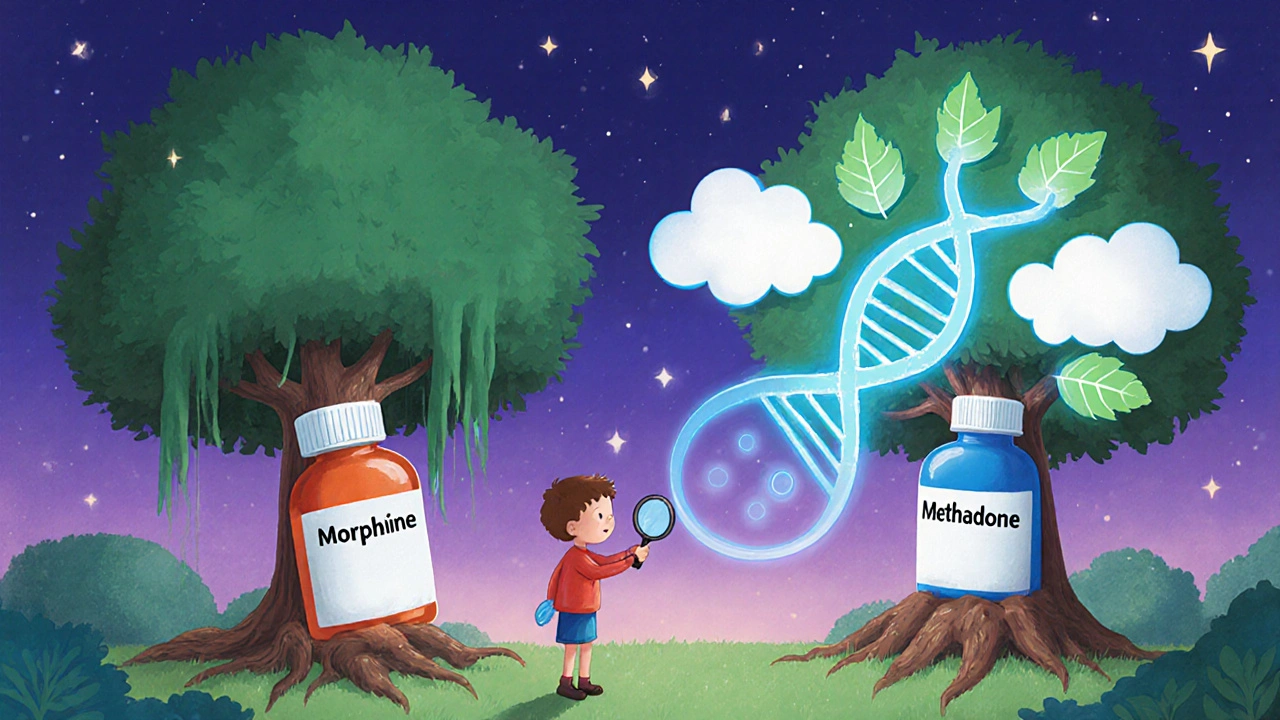
- Methadone: The standout. It often lets patients reduce their total daily dose significantly-sometimes by 30-50%. Why? Methadone works differently. It blocks pain receptors and also affects another brain pathway (NMDA receptors) that helps reduce nerve sensitivity. Plus, recent studies suggest the old conversion ratios (like 3:1 or 5:1 morphine to methadone) are too high. The real ratio for side effect reduction might be closer to 9:1 or even 10:1.
But here’s the catch: methadone is tricky. It builds up in the body over days. If you switch too fast or don’t reduce the dose enough, you can overdose. That’s why it’s never done without close monitoring.
Equianalgesic Dosing: The Math Behind the Switch
You can’t just swap one opioid for another at the same dose. That’s dangerous. The body handles each drug differently. That’s where equianalgesic dosing comes in-the process of calculating an equivalent pain-relieving dose between opioids.But here’s the problem: those tables aren’t perfect. They’re based on averages. Your body might metabolize drugs faster or slower due to genetics, age, liver function, or even what you ate that day. That’s why most guidelines recommend reducing the new opioid’s dose by 25-50% when switching-especially if you’ve been on high doses for a long time. This accounts for something called “incomplete cross-tolerance.” Your body isn’t fully used to the new drug, even if you’re used to the old one.
For example: if you were on 120 mg of morphine daily, a standard conversion table might say that’s equal to 40 mg of oxycodone. But to be safe, your doctor might start you at 20-30 mg instead. Then, after a few days, they’ll slowly adjust upward if needed. This isn’t being cautious-it’s standard practice.
What About Methadone’s Dose Drop?
Methadone is the exception that proves the rule. In outpatient palliative care studies, patients who switched to methadone consistently ended up with lower Morphine Equivalent Daily Doses (MEDD). Other opioids? Not so much. Most rotations didn’t lower total daily doses. But methadone did. Why?Because methadone isn’t just another opioid. It’s a double-action drug. It binds to mu-opioid receptors (like morphine) but also blocks NMDA receptors, which are involved in chronic pain signaling. This means it can control pain more efficiently-sometimes with less total drug. That’s why it’s often chosen for patients who’ve hit the ceiling with other opioids.
But again-methadone isn’t a magic bullet. It has a long half-life. It can stay in your system for days. That means if you switch too quickly, you could accidentally overdose. That’s why it’s only done in settings where doctors can monitor you closely, especially in the first week.
Why Are There No Big Clinical Trials?
You’d think, with so many people using this approach, there’d be a massive, randomized trial proving it works. There isn’t. Most of the evidence comes from observational studies-tracking patients over time, not comparing groups in controlled settings.That’s a gap. Experts admit it. The 2009 guidelines were based on expert consensus, not gold-standard trials. And even now, in 2025, there’s still no large study showing whether opioid rotation improves long-term outcomes like quality of life or hospitalizations.
But here’s the thing: in clinical practice, when patients are stuck-when they’re vomiting every morning, or can’t get out of bed because they’re too sleepy-the risk of doing nothing is higher than the risk of switching. That’s why it’s still widely used. It’s not perfect. But it’s often the best option left.
What’s Next for Opioid Rotation?
The future is personalization. Researchers are looking at genetic testing to predict how someone will respond to certain opioids. Some people have gene variants that make them process codeine too quickly (turning it into dangerous levels of morphine). Others metabolize oxycodone too slowly, meaning they don’t get relief. In the next few years, we may see doctors use a simple cheek swab to guide opioid choices-before the patient even starts.Electronic health records are also getting smarter. Some hospitals now have built-in alerts that flag when a patient is on a high dose or has had multiple rotations. They suggest safe conversion ratios and flag potential interactions. That’s huge. It means fewer mistakes.
For now, though, the best tool is still a careful, thoughtful conversation between patient and provider. Not every side effect needs a switch. Sometimes, adding a laxative or anti-nausea med is enough. But if you’ve tried that and still feel awful-opioid rotation might be your next step.
What Patients Should Know Before Starting
If your doctor suggests a switch:- Ask: Why this drug? What side effects am I hoping to avoid?
- Ask: What’s the starting dose, and why? Will I be monitored closely?
- Ask: What signs should I watch for? When do I call if something feels wrong?
- Don’t assume the new drug will work instantly. It can take 3-7 days to stabilize.
- Keep a pain and side effect diary. Note what you feel each day. That helps your doctor adjust faster.
This isn’t a one-time fix. It’s part of ongoing pain management. And it’s okay to try more than one rotation if the first doesn’t work. Many patients end up trying two or three different opioids before finding the right fit.
Is opioid rotation safe?
Yes, when done correctly. The biggest risk is overdose, which can happen if the new opioid dose is too high or if cross-tolerance isn’t accounted for. That’s why experts recommend reducing the new dose by 25-50% when switching, especially after long-term or high-dose use. Always do this under medical supervision.
Can I switch opioids on my own?
No. Never switch opioids without your doctor’s guidance. Even small changes in dose can be dangerous. Different opioids have different half-lives, metabolisms, and safety profiles. A mistake can lead to respiratory depression, coma, or death.
Does opioid rotation mean I’m addicted?
No. Addiction is about compulsive use despite harm. Opioid rotation is a medical strategy to improve safety and effectiveness. It’s no different than switching from one antibiotic to another when the first doesn’t work. It’s about finding the right tool for your body.
How long does it take to feel better after a switch?
It varies. Pain relief may improve within a few days, but side effects like nausea or drowsiness can take up to a week to fully resolve. Methadone can take longer-up to 10 days-to reach steady levels in your system. Patience and close monitoring are key.
Will I need to keep rotating opioids forever?
Not necessarily. Many patients find one opioid that works well and stay on it for years. Others may need to rotate again if their pain changes or new side effects appear. It’s not a failure-it’s part of managing a complex condition. The goal is sustainable, tolerable pain control-not a perfect, lifelong solution.






9 Comments
So... let me get this straight: they’re swapping one mind-altering chemical for another... but it’s ‘smart’? 🤔 You know what else was ‘smart’? The pharmaceutical industry convincing doctors that opioids were ‘safe’ in the 90s. Now we’ve got whole generations hooked on a revolving door of pills that all do the same thing-just with different brand names and slightly different side effect brochures. I’m not saying don’t rotate-I’m saying the whole system is a rigged casino, and we’re just betting on which slot machine won’t steal your soul first.
This is so important!! 💗 I switched from morphine to oxycodone after 3 years of constant vomiting and brain fog-and within a week, I was cooking again, laughing with my kids, actually sleeping at night. It’s not about addiction-it’s about dignity. 🙏 If your doctor won’t listen, find one who will. You deserve to live, not just survive.
The clinical evidence supporting opioid rotation is robust within palliative and chronic pain management circles, despite the absence of large-scale randomized controlled trials. The ethical imperative to mitigate suffering outweighs the methodological limitations of observational data. The pharmacodynamic variability among opioids is well-documented in peer-reviewed literature, and the practice of dose reduction during rotation is standard of care. To dismiss this as anecdotal is to ignore the lived reality of millions who experience tangible, life-improving outcomes.
It is imperative to underscore that opioid rotation, when conducted under the supervision of a qualified pain management specialist, constitutes a medically sound and ethically defensible intervention. The notion of ‘opioid resistance’ is a misnomer that perpetuates stigma and impedes optimal therapeutic outcomes. As evidenced by the Journal of Pain and Symptom Management guidelines, the focus must remain on pharmacological individualization-not patient blame. This approach aligns with the foundational principles of patient-centered care.
Oh wow, so now we’re pretending methadone’s some kind of magic bullet? LOL. You know what else they said was a ‘game-changer’? OxyContin. ‘Less addictive!’ they said. ‘Better pain control!’ they said. Now half the country’s on fentanyl patches and half the other half is on methadone clinics. And guess what? The death rates didn’t drop-they just moved from one drug to another. And don’t even get me started on how the conversion ratios are basically guesswork based on white male bodies from the 80s. My cousin’s 72-year-old grandma with liver cirrhosis got switched using those tables? She ended up in ICU. This isn’t science-it’s pharmaceutical roulette with a side of paternalism.
Equianalgesic tables are statistically invalid. Cross-tolerance is poorly quantified. Methadone’s NMDA antagonism is overhyped. The real issue is polypharmacy and inadequate non-opioid adjuvants. You need gabapentinoids, SNRIs, and neuromodulation-not more opioids. Rotation is a band-aid on a hemorrhage.
Why are we even talking about this? In India, we don’t waste time with fancy rotations. If you can’t handle pain, you’re weak. We have turmeric, yoga, and discipline. This Western opioid obsession is a disease of the soft. Stop whining. Get stronger.
Let’s be real-this whole opioid rotation narrative is just the latest chapter in the Great Pharmaceutical Manipulation. They don’t care if you live or die-they care if you keep buying. Morphine? Sold. Oxycodone? Sold. Methadone? Sold. Fentanyl patch? Sold. Every time you ‘rotate,’ you’re feeding the machine. And who profits? The same corporations that funded the studies, wrote the guidelines, and lobbied the FDA. They’re not healing you-they’re harvesting your dependency. You think this is medicine? It’s capitalism with a stethoscope.
There’s a quiet tragedy in all of this: we’ve turned pain into a problem to be solved with chemistry, rather than a human experience to be witnessed. Rotation may alleviate symptoms, but it doesn’t address isolation, trauma, or the erosion of meaning that often accompanies chronic suffering. We treat the body like a machine, forgetting that the soul also aches-and no pill, no matter how cleverly rotated, can heal that.