TL;DR
- Enteric infections can disrupt the gut microbiome, weakening oral tolerance and raising food allergy risk.
- Both bacterial (e.g., Clostridioides difficile is a gram‑positive anaerobe that causes severe colitis) and viral (e.g., Rotavirus is a double‑stranded RNA virus that targets intestinal cells) infections have distinct immune signatures.
- Key immune players-Th2 cells, IgE, IL‑4, and IL‑13-drive the allergic cascade after gut barrier damage.
- Early‑life antibiotic exposure, poor diet, and a hygiene‑driven microbiome deficit amplify the problem.
- Probiotic and prebiotic interventions show promise for restoring tolerance, but timing matters.
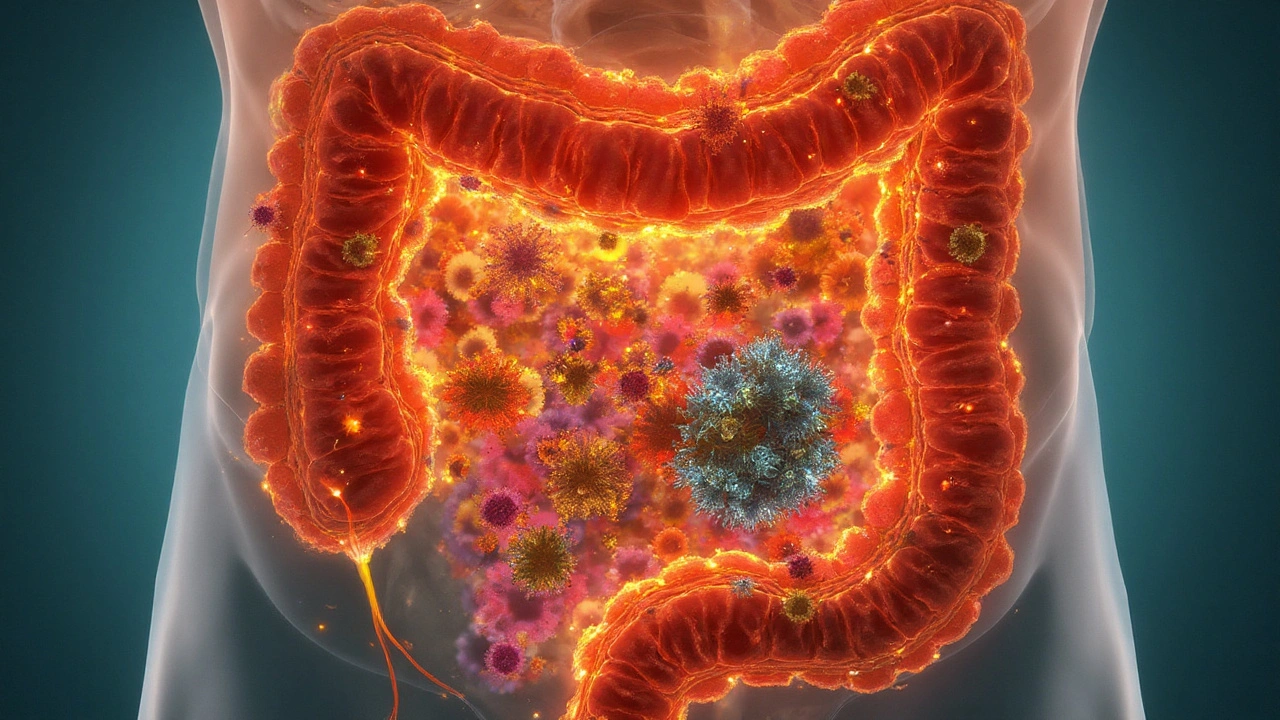
What Are Enteric Infections?
Enteric infection is a gastro‑intestinal disease caused by pathogenic bacteria, viruses, or parasites that invade the intestinal tract, leading to inflammation, diarrhoea, and sometimes systemic effects. In the UK alone, over 2million cases are reported each year, with children under five accounting for 30% of admissions. The infection’s impact goes beyond acute illness; emerging data link it to chronic immune dysregulation, especially food‑related hypersensitivity.
Food Allergies: A Growing Public‑Health Concern
Food allergy is a IgE‑mediated immune reaction that occurs when the body mistakenly identifies a harmless food protein as a threat, triggering symptoms ranging from itching to anaphylaxis. Recent UK prevalence estimates put the figure at 8% of children and 3% of adults, showing a steady rise over the past two decades. The mystery: why are more people developing these reactions now?
How the Gut Microbiome Connects Infections to Allergies
Gut microbiome is a complex community of bacteria, fungi, viruses, and archaea living in the gastrointestinal tract, essential for digestion, vitamin synthesis, and immune education. A balanced microbiome teaches the immune system to ignore harmless antigens-a process called oral tolerance. When an enteric infection wipes out key commensals (e.g., Bifidobacterium and Lactobacillus species), the tolerance‑inducing signals weaken, leaving the gut vulnerable to allergic priming.
Immune Pathways That Turn Infection Into Allergy
Three mechanisms dominate the transition:
- Barrier disruption: Inflammation loosens tight junctions, allowing larger proteins to cross the epithelium and meet immune cells.
- Th2 skewing: Certain pathogens stimulate a Th2 immune response, releasing cytokines like IL‑4, IL‑5, and IL‑13 that promote IgE class switching.
- Regulatory T‑cell (Treg) depletion: Healthy microbes foster Tregs that suppress hypersensitivity; infection‑driven dysbiosis reduces their numbers.
For instance, a 2023 cohort study showed that children hospitalized with Clostridioides difficile infection had a 2.4‑fold higher odds of developing a new food allergy within two years compared to matched controls.
Comparing Bacterial and Viral Enteric Infections
| Attribute | Bacterial (e.g., C. difficile) | Viral (e.g., Rotavirus) |
|---|---|---|
| Typical immune shift | Strong Th2 bias, high IL‑4/IL‑13 | Mixed Th1/Th2, transient IL‑10 surge |
| Gut barrier effect | Severe tight‑junction loss | Moderate, often reversible |
| Microbiome disruption | Profound loss of Firmicutes | Short‑term dysbiosis, rapid recovery |
| Allergy risk increase (2‑yr follow‑up) | 2.4× | 1.6× |
The table highlights why bacterial infections, especially those requiring antibiotics, tend to leave a longer‑lasting imprint on allergy development.

Antibiotics, Hygiene, and the ‘Missing Microbes’ Hypothesis
When physicians prescribe broad‑spectrum antibiotics for an infection, they unintentionally wipe out beneficial microbes. A 2022 meta‑analysis of 45 studies linked early‑life courses of three or more antibiotic courses to a 30% rise in food allergy incidence.
Coupled with modern hygiene practices, the effect mirrors the classic “hygiene hypothesis”: reduced exposure to environmental microbes limits the immune system’s opportunity to learn tolerance, making it over‑reactive to harmless food proteins.
Can Probiotics or Prebiotics Reverse the Damage?
Interventions aimed at restoring a healthy microbiome are gaining traction. Two key players:
- Probiotic therapy: Strains such as Lactobacillus rhamnosus GG have been shown in randomized trials to lower the odds of developing a new peanut allergy when administered during the first six months after a severe gastroenteritis episode.
- Prebiotic supplementation: Non‑digestible fibers (e.g., inulin, GOS) feed native bifidobacteria, encouraging short‑chain fatty acid production that strengthens the gut barrier.
Timing matters. A 2024 study demonstrated that starting probiotic treatment within 48hours of infection reduced IgE levels by 15% compared to delayed initiation.
Practical Steps for Parents and Clinicians
- Monitor children after any severe diarrhoeal illness for signs of emerging food sensitivities (skin rashes, hives, gastrointestinal distress).
- Limit unnecessary antibiotics; consider narrow‑spectrum agents when treatment is essential.
- Introduce age‑appropriate probiotic supplements promptly after infection, following pediatric guidance.
- Encourage a diet rich in fermented foods (yogurt, kefir, kombucha) to naturally repopulate beneficial microbes.
- When a new allergy is suspected, perform specific IgE testing early to guide dietary management.
These actions address both the immediate aftermath of infection and the longer‑term trajectory toward tolerance.
Related Concepts Worth Exploring
The discussion of enteric infections and food allergies opens doors to several adjacent topics, such as:
- Eosinophilic esophagitis - a chronic, allergy‑driven condition of the oesophagus linked to early gut inflammation.
- Oral tolerance induction protocols - therapeutic desensitisation used in allergy clinics.
- IL‑4 and IL‑13 blockers - biologic drugs currently approved for atopic dermatitis that may impact food allergy pathways.
- Gut‑brain axis - how intestinal inflammation can affect neuro‑immune signalling and possibly exacerbate allergic behaviours.
- Fecal microbiota transplantation (FMT) - experimental approach to reset the microbiome after recurrent infections.
Readers interested in the broader ecosystem of immune‑gut interactions can dive into these areas for a richer understanding.
Future Directions in Research
Scientists are now leveraging longitudinal birth‑cohort studies combined with metagenomic sequencing to pinpoint which bacterial species protect against allergy after infection. Early results suggest that restoring a specific cluster of Clostridia may re‑establish Treg populations and lower IgE production.
Clinical trials are also testing next‑generation probiotics engineered to secrete IL‑10 directly in the gut, a promising strategy to counteract Th2 skewing in real time.

Frequently Asked Questions
Can a single bout of gastroenteritis cause a lifelong food allergy?
A single severe infection doesn’t guarantee an allergy, but it can tip the immune balance. Children who experience intense gut inflammation combined with antibiotic use have a markedly higher risk of developing a new allergy within the next few years. Early intervention with probiotics may reduce that likelihood.
Are viral infections less risky than bacterial ones for developing food allergies?
Generally, bacterial infections-especially those requiring broad‑spectrum antibiotics-pose a greater risk because they cause deeper microbiome disruption and stronger Th2 skewing. Viral infections can still contribute, but the effect tends to be milder and more transient.
Should I give my child probiotic supplements after every stomach bug?
It’s worth discussing with a paediatrician. Evidence supports probiotic use within 48hours of a serious infection, particularly for strains shown to aid tolerance. Routine use after mild, self‑limiting diarrhoea isn’t universally recommended.
How do antibiotics increase the chance of a food allergy?
Antibiotics wipe out beneficial gut bacteria that train the immune system to ignore food proteins. This loss reduces regulatory T‑cell numbers, weakens the gut barrier, and allows allergen‑specific IgE to form more easily.
Is there any test to predict who will develop a food allergy after infection?
Currently, no single test predicts it reliably. Researchers are exploring stool metagenomics and serum cytokine panels, but for now clinicians rely on family history, severity of the infection, and early IgE screening when symptoms arise.




11 Comments
Man, I had a crazy stomach bug last year and then suddenly couldn't eat peanut butter anymore. Didn't connect the dots until I saw this post. Scary how one infection can change your whole life.
Let’s not reduce this to mere pathophysiology - the gut is not just a pipe for nutrients, it’s a sentient ecosystem, a living archive of evolutionary negotiation between host and microbe. When we obliterate Bifidobacterium with antibiotics, we’re not just killing bacteria - we’re erasing epigenetic memory encoded in microbial metabolites that taught our Tregs to recognize soy as ‘self.’ The Th2 skew isn’t a bug - it’s a failure of microbial diplomacy. And let’s be real: our sanitized, ultraprocessed, screen-staring, antibiotic-sprayed modernity has turned our immune systems into overzealous bouncers at a club they’ve never seen before.
Probiotics? Maybe. But only if they’re not just generic L. rhamnosus GG from a Walmart shelf - we need strain-specific, host-matched, metabolite-optimized consortia. And prebiotics? Inulin is fine, but what about resistant starches from green bananas or plantains? That’s ancestral fuel. We’re treating symptoms, not restoring the ancestral contract between microbiota and mucosa.
And don’t get me started on FMT - it’s not fecal transplants, it’s microbial resurrection. We’re not transplanting poop, we’re transplanting a lost civilization. The real tragedy? We’re trying to fix this with pills while the world keeps sterilizing everything - from baby bottles to playgrounds. We’ve forgotten that dirt isn’t the enemy - ignorance is.
This is the most important public health insight in a decade and nobody’s talking about it. We’re spending billions on allergy meds while ignoring the root cause: our gut is dead because we’ve been living like lab rats in a sterile bubble. Kids need to eat dirt, play with dogs, and stop being sterilized at birth. Probiotics aren’t a supplement - they’re a rescue mission. And if you’re waiting for your pediatrician to tell you what to do, you’re already behind. Start with soil-based probiotics and fermented veggies. Don’t wait for a diagnosis - prevent it. This isn’t science fiction, it’s evolutionary biology. We’re not broken - we’re just out of touch with the microbes that made us.
I’ve been reading up on this since my daughter had rotavirus at 8 months and then developed an egg allergy. It makes so much sense now - the timing lined up perfectly. I started her on a pediatric probiotic within 48 hours after the illness, as the article suggested, and honestly? No new allergies since. I know it’s anecdotal, but it’s the only thing that felt like we actually did something right. I wish more doctors talked about this instead of just handing out epipens.
i read this and thoguht about my kid who got sick after day care last year and now cant eat milk… is this why? i dont know if i got the right probiotic or not… sorry for typos im on my phone
So let me get this straight - you’re telling me the real reason kids are allergic to peanuts is because we washed our hands too much? Next you’ll say vaccines cause autism because we didn’t let our kids play in goat feces
The data is correlational, not causal. Antibiotic use correlates with both infections and allergies - but is it the antibiotics or the underlying severity of illness? Confounding variables like socioeconomic status, diet, and access to care aren’t adequately controlled in most studies. Also, ‘microbiome disruption’ is a buzzword that means different things to different people. Until we have longitudinal metagenomic data with functional validation, this remains speculative.
While the hypothesis is compelling, the methodology of the cited cohort study is questionable. The control group was matched for age and sex, but not for feeding practices, household pet exposure, or maternal microbiome status during pregnancy - all significant confounders. Furthermore, the 2.4-fold increase sounds alarming, but without absolute risk figures, it’s misleading. If baseline risk is 0.5%, then 1.2% is still a very small absolute increase. This is classic fear-mongering disguised as science.
THIS IS ALL A PHARMA SCAM. They want you to buy probiotics so they can sell you allergy meds later. The real cause? Glyphosate in your food. The CDC knows. The WHO knows. But they won’t tell you because Big Pharma owns the FDA. Your gut isn’t broken - it’s poisoned. Stop taking their pills and eat organic kale. Also, rotavirus vaccines were designed to create more allergies so they could sell more epipens. Look it up.
Thank you for this meticulously referenced and clinically grounded summary. The distinction between bacterial and viral etiologies in immune skewing is particularly well-articulated. I will be incorporating these insights into my upcoming lecture series on pediatric immunology. The emphasis on timing of probiotic intervention is critical - it aligns with recent findings in mucosal immunology regarding the narrow window of immune plasticity post-infection. A truly valuable contribution to the field.
I appreciate how balanced this is. I’ve seen too many posts that either panic people or dismiss the whole thing. The practical steps at the end? Perfect. Especially #2 - limiting antibiotics. My doctor was shocked when I asked if a narrow-spectrum option was possible after my son’s stomach bug. He said most parents just want the ‘strongest’ one. We need more awareness like this.